Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.16 no.2 Ciudad de México abr./jun. 2012
Case reports
Multi-disciplinary prosthetic rehabilitation. Clinical case report
Susana Mendoza Rivera,* Enrique Ríos Szalay,§ Alejandro Treviño Santos,§ Selene Olivares TapiaII
* Student, Oral Prostheses Specialty, Graduate School.
§ Professor, Oral Prostheses and Implantology Specialty, Graduate School.
II Student, Periodontics Specialty, Graduate School.
National School of Dentistry, National University of Mexico, UNAM.
ABSTRACT
In present days, evolution in Dentistry and changes in prosthetic techniques and materials have rendered patients more demanding in matters concerning aesthetics, function, and comfort. Issues involving face and teeth require interaction of several dental disciplines, with the aim of attaining prevention, function and aesthetics, which can be attained through well organized communication. Multidisciplinary prosthetic rehabilitation meets that goal. A multidisciplinary treatment is based upon diagnosis, planning and therapeutic procedures.1,2 Treatment planning can initiate with a visualization of the final result. If several disciplines were not to be involved in the comprehensive treatment, results could result compromised.3 Objective: Step by step description of clinical phases, in a multidisciplinary treatment based upon diagnosis and planning. Different specialties are involved: Surgery, Implantology, Periodontics, Endodontics, Oral Prosthetics and Occlusion. The inclusion of all these disciplines will achieve stability in the periodontal tissues as well as tissues surrounding future implants, recovery of periodontal architecture and masticatory function, as well as attaining acceptable aesthetic results and gaining the patients aesthetic and functional satisfaction. Clinical case presentation: 47 year old female patient, in general good health, some missing teeth, inappropriate prosthetic work, loss of periodontal support as well as aesthetic and functional alterations. Treatment plan was decided upon, and divided into four phases: the first phase consisted on tooth extraction and implant placement. The second phase involved canal treatment and re-treatment with stump reconstruction, which involved the making of a guide for partial coronary conformation. The third prosthetic phase involved treatment of soft tissues, impressions, implant rehabilitation, characterization, cementing with the CAD-CAM Procera ® system and occlusal splint. The fourth phase involved periodontal and prosthetic control. Conclusion: Treatment success was based upon the following factors: 1) Maintenance of periodontal and tissues surrounding the implant, 2) Periodontal architecture recovery, 3) Masticatory function recovery, 4) Obtaining acceptable aesthetic results, 5) Patient's satisfaction with respect to aesthetics and function.
Key words: Prosthetic rehabilitation, multidisciplinary diagnosis, planning and communication, multidisciplinary treatment, state-of-the-art prosthetic materials and techniques (dental implants CAD/CAM system), fiber-reinforced posts.
INTRODUCTION
The intent of multi-disciplinary prosthetic rehabilitation is to conduct a comprehensive treatment, where different dental disciplines are involved, with the goal of accomplishing an ideal case of prevention, function and aesthetics.
A multi-disciplinary team is described as a set of individuals with varied academic background and professional experience, who operate together for a pre-established period aiming at solving some complex problem. That is to say, they have a common goal. Each individual is conscious of his role as well as the role of others; they work as a team under the direction of a coordinator.4
In our days it is very frequent to find cases where a multi-disciplinary rehabilitation is required. This comprehensive treatment can include emergency endodontic or periodontal treatment to preserve remaining dental or periodontal structures, as well as gaining aesthetic and functional morphologic rehabilitation.5 A multi-disciplinary treatment not only confers the opportunity to change the approach of a dental treatment, it can develop and shape the physical appearance of a subject and simultaneously provide restorations that are aesthetic, durable and functional.
It is important to single out patients concerns and requirements, and assess whether, as a specialist, one is able to solve the problem. If this is not the case, help from another specialist must be sought to reach good results and patient improvement. The key to success is to use a type of methodology which, step by step, structures treatment options before deciding upon a definite plan and developing multidisciplinary relationships.6
Multidisciplinary rehabilitation encompasses the combination of diagnosis, treatment planning as well as therapeutic procedures. It is of foremost importance for the rehabilitating clinician to select a proper working team, since the process of selection can bear positive or negative influence into the global treatment. Each caregiver in the team must possess an optimum skill level in his area of specialty. He can then become a positive factor6 and achieve an overall vision of the problem as well as the coordinated intervention of several advanced technology specialties tailored to the different problems encountered in these clinical cases.
When performing a multidisciplinary prosthetic rehabilitation, one of the main therapeutic goals is to preserve, inasmuch as possible, remaining natural dentition. Currently, dental implants play a very important role in the creation of new treatment options. Another fact to be recognized is that specialists, laboratory technicians and patients work as a team every day to try to solve certain qualitative and quantitative difficulties encountered in treatments.7,8 For example, could a tooth be endodontically treated, and after that restored with a prosthesis, or be extracted and replaced with a fixed prosthesis or a crown supported by an implant? Several alternatives have been considered and discussed, but results are limited.9-11 Available reviews do not compare all accessible alternative treatments, and neither are all possible results to those treatments taken into consideration.12,13
Endodontic therapy has awarded the dentist the possibility of preserving teeth which otherwise might have been extracted. The extent of crown destruction and the type of tooth will determine the type of restoration to be used on an endodontically treated tooth. The decision of placing an intra-radicular reconstruction is based upon parameters such as position of the tooth in the arch, occlusion, function of the restored tooth, amount of remaining dental structure, root canal configuration and supporting tissues characteristics.14,15
In our days, it is considered that the placement of endodontic posts has the single aim of providing retention to the final restoration.16 Tooth resistance to fracture is directly related to the amount of remaining tissue. This resistance decreases due to the accumulated loss of tooth structure caused by endodontic and restorative procedures.
Roblee & al. showed that endodontic procedures reduce tooth rigidity in only 5%, whereas preparation of a Class IV cavity reduces rigidity in 60%. From this we can understand that resistance decrease in endodontically treated teeth is mainly due to the loss of crown structure as opposed to endodontic treatment per se. 16
Clinical options for the restorations of anterior teeth are dictated by present alterations as well as aesthetic and functional demands. Retrospective studies conducted on posterior teeth having received root canal treatment, indicate there is higher probability of fracture in instances when they are not covered with crowns. A splint effect is achieved when 1 to 2 mm axial vertical structure is covered within the restoration walls, thus protecting the tooth against fractures.17
It has been observed that periapical health depends significantly more on the restoration than on the endodontic treatment. Contamination of root canals can occur during as well as after restoration of endodontically treated teeth. It is therefore of utmost importance to take into account general standards to decrease factors which might cause failure of endodontic treatment and consequently, lack of success of the restorative treatment.18
The introduction of materials able to adhere to dentin has created the potential opportunity of reconstructing and rehabilitating lost dental tissues and thus save extensively damaged teeth. Due to their sufficient strength, composite resins have been widely accepted as reconstructive material. The use of light-transmitting fiber posts combined with adhesive materials represents a conservative rehabilitation technique.19
Aesthetic appearance achieved through a restorative treatment is a byproduct of several dental procedures which involve occlusion analysis, orthodontic movement, conservative and restorative periodontic treatment, oral surgery, and bone integrated implants.
CLINICAL CASE
47 year old female patient lacking medical history that might preclude dental treatment. The patient was referred from a general dentistry clinic to the Graduate and Research School of the National School of Dentistry, National University of Mexico (UNAM) to be considered for multidisciplinary treatment. The reason behind the consultation was replacement of missing teeth with implants and improvement of aesthetics.
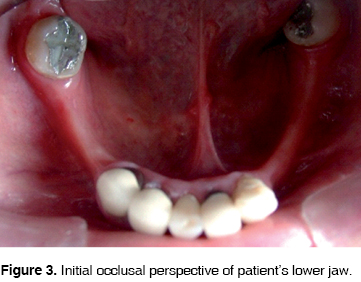
Dental exploration revealed the following: absence of teeth number 18, 17, 27, 28, 33, 34, 35, 36, 38, 44, 45, 46, and 48. Approximately five years previously, metal-porcelain individual crowns had been placed in teeth number 15, 14, 13, 12, 11, 21, 22, 23, 24, 25, 31, 42 and 43. Teeth 3, 16 had a metallic onlay. Amalgams could be found in the occlusal sides of teeth 37 and 47. Tooth 26 presented a stump with miracle-mix, and in the lower jaw, there was a long standing, flexible, removable partial prosthesis. Any other exact data were lacking (Figures 1, 2 and 3).


When undertaking periodontal examination of the upper jaw, the following was observed: recessions, lack of inter-dental papillae conformation, a 2 to 3 mm probing depth as well as tattoos in the left ridge.
A Kennedy Class III edentulous gap was observed in the lower jaw; with remnant teeth showing grade 2 mobility, loss of bone support and swelling in edentulous zone (Figure 4).

Endodontic evaluation showed hypersensitivity to thermal changes in teeth number 41 and 32. The patient informed that approximately 10 years before she underwent canal treatment in all teeth having now metal-porcelain crowns.
With the aid of the orthopantomography the following was observed: absence of many teeth, adequate root-crown relationship, horizontal and vertical mandibular bone loss, canal treatment in upper jaw teeth and maladjusted crowns (Figure 5).

Based on the aforementioned data, the following diagnosis was emitted: Patient partially edentulous, Kennedy Class III in lower jaw, with grade II dental mobility in anterior teeth, loss of bone support in edentulous zone. Periapical reactions in sites where canal treatment had been performed. Poorly adjusted individual restorations. Decrease of vertical dimension due to absence of posterior teeth. Functional problems hindering proper feeding as well as inadequate aesthetics.
Treatment was planned into four phases: The first phase consisted of lower molars extraction and placement of implants, the second phase covered treatment and re-treatment of root canals, with stump rebuilding; this implied production of a guide for partial coronary conformation. The third phase was of a prosthetic nature: soft tissue management with temporary appliances impression taking, implant rehabilitation, characterizations, cementing with CAD-CAM Procera ® system and occlusal splint. The fourth phase consisted in periodontal and prosthetic control.
FIRST PHASE
In a first surgical phase, five IMTEC® conventional load implants were placed in the lower jaw edentulous area (4 mm diameter for molars and 3.75 mm for premolars) for a period of approximately 8 months, to prepare for the second surgical phase where healing screws could be placed (Figure 6).
At the point in time when the reconstruction device was removed, tooth number 26 presented communication with the furcation. In joint consultation with the Periodontics Department, it was decided to perform an atraumatic extraction as well as collation of bone and connective tissue graft to prepare for a future implant in three months time.
Once the implants were integrated into the bone and provisional removable partial prosthesis was devised to preserve vertical dimension, teeth number 37 and 47 were extracted.
Before the completion of bone integration, a left lower implant presented apical reaction. After joint consultation with the maxillofacial surgeon, removal of the implant was performed and a course of antibiotics administered.
SECOND PHASE
All existing porcelain-metal crowns were removed: 15, 14, 13, 12, 11, 21, 22, 23, 24, 25, 31, 42, and 43, along with metallic posts. Provisional work was performed with Lang s Jet Tooth Shade ® self-curing acrylic resin, care being taken not to modify existing vertical dimension and shape, as well as preserving fit and gingival architecture (Figures 7 and 8).

Once completed the provisional measures for the whole lower jaw, a silicone impression was taken (with the system of light-heavy addition) with Elite H-D Zhermack ® polyvinyl siloxane. Clips were used within the root canals to transport all residual and marginal information as well as obtaining a working model to manufacture a reconstruction guide.
For the creation of the plaster Elite Rock type 4 Zhermack ® gypsum model, all reconstructions were waxed and with the aid of an electric micro-burr device ( Microfresadora APF 450 ® ) an adequate parallelism was established as forerunner for future crown insertion. After this procedure, a flexible acetate guide was obtained to manufacture provisional teeth (Figure 9)
The patient was remitted to the Endodontics Department for root canal treatment and re-treatment. Once this regimen was completed, glass fiber posts reinforced with FRC Postec Plus ® (Ivoclar, Vivadent ) were placed. These posts were cemented with flow reconstruction resin used for adhesive cementation of endodontic fiber reinforced posts Multicore Flow (Ivoclar Vivadent).
Cemented posts were reconstructed with Multicore HB (Ivoclar Vivadent) heavy body resin to be later conformed with the acetate reconstruction guide (Figure 10)

With the aid of diagnosis waxing new provisional teeth were manufactured. This procedure modified vertical dimension (Figure 11).

THIRD PHASE
The following procedure was conducted: soft tissue management with provisional teeth, impressions, implant rehabilitation, characterizations, system CAD-CAM Procera ® cementing, and placement of occlusal splint.
Preparations taken in the mouth were obtained using Elite H-D Zhermack polyvinyl-siloxane, to ascertain insertion ways in a work model with the aid of a parallelometer and perform adjustments in the mouth. Once the preparations performed in the mouth were retouched, final impression was taken with the double thread and following a two phase impression technique, using as material Elite H-D Zhermack polyvinyl siloxane (Figure 12).
In the lower jaw, due to the presence of implants, final impression was taken with Impregnum 3M ESPE polyether with open tray. Residual teeth impressions were taken with the double thread technique.
EPS Laboratorio Dental prosthetic dental laboratory sent work models to conduct transportation to the semi-adjustable Hanau articulator. The aforementioned laboratory included as well thermo-curing acrylic resin guides for the recording of centric relation and vertical dimension (Figures 13 and 14).

Gold carved devices of the four bone-integrated implants were tested (Figure 15).
During this phase, tooth number 14 presented periapical reaction. For this reason, and jointly with the Periodontics department, it was decided to place an immediate load implant. An immediate load 3i implant was placed in the molar zone of tooth number 26. A restricted surgical guide was manufactured (Figure 16 and 17).
Resin copings were tested in the upper jaw in order to manufacture zircon Procera ® crowns. In the lower jaw a metallic substructure was fit for two fixed prostheses supported by implants and with mesial cantilever in both. Resin copings in the anterior section showed good fit (Figure 18).
The laboratory sent the test models (biscuit porcelain test) back. Prosthetic corrections regarding shape and occlusion were performed previous to finally sending all Procera® with Relay X Unicem (3M ESPE) crowns to be glazed and cemented (Figure 19).

In the lower jaw, both prostheses supported by implants were manufactured in gold-ceramic, with mesial cantilever, and were cemented with Relay X Unicem (3M ESPE) .
Final cementation and final Orthopantomography (Figures 20, 21 and 22).



Occlusal splint (Figure 23).

FOURTH PHASE
Periodontal, prosthetic and radiographic control one year after procedure (Figures 24 and 25).


DISCUSSION
Based upon a comprehensive diagnosis, it is possible to offer prosthetic conventional treatment, as well as with implants, to restore function and aesthetics. Since the introduction of bone-integration practices, treatment predictability has been extended up to the point of incorporating them into present standard treatments. Success rate at 8 and 10 years has been 90%. Restoration involving implants offer a greater predictable advantage over fixed partial prostheses when replacing a missing tooth.20
Some patients are intolerant to prostheses. Others experiment psychological disorders when using removable prostheses, and possess sufficient bone volume. In these cases, patients can opt for implants, as another treatment alternative to replace lost dentition.21,22 Implants are indicated for patientes with compromised dentition requiring full rehabilitation.23,24
Periodontal treatment plays an important role and is essential for any multidisciplinary treatment plan.
New fiber glass endodontic posts are a good alternative to preserve and rehabilitate endodontically treated teeth; characteristics of these devices lead to a positive prognosis.25
FRC Postec Plus ® is a fiber glass reinforced post system. It offers high radio-opacity, which can be deemed similar to that of metallic posts. With these devices, radio-opacity reaches high levels and can be clearly identified in x-rays.
Multicore HB ® is a self-curing resin material used for nuclei. Optionally, it can be light-cured; it provides optimum base for the reconstruction of vital and non vital teeth which might have partially or entirely lost their clinical crown. This material can be mixed, as well as conveniently modeled and applied with appropriate instruments. Total polymerization time for this material is 4-5 minutes. This allows to actively control the polymerization process, since it can be additionally exposed to light (40 seconds to each side).
MultiCore Flow ® is a cement offering flow consistency for adhesive cementation of fiber glass reinforced endodontic posts such as FRC Postec Plus ® The cartridge system with intra oral points self mixing cannula, ensures rapid mixing of the material and allows for an accurate application. MultiCore ® adapts very well to dentinal surfaces previously treated with adhesive agents. It provides solid adhesion to remaining dental tissue. The material is self-etching. Concurrently with the adhesive agent AdheSE ® , Multicore ® forms a coordinated system which yields adequate, easy to replicate results. Nevertheless, it is well understood, that well recognized and tested materials such as Syntac, Excite, and Excite DSC (Ivoclar Vivadent) can be equally used.
Properly adapted and modeled provisional restorations can be used as templates for permanent restorations. They must protect the prepared dental structure and as well maintain the position of the tooth in the arch. Fit is vital when margins are left in subgingival position, since, if a space is generated, in the case when the margins are left short, gingival tissues can proliferate and penetrate into any opening of the acrylic material. If the provisional restoration lacks sufficient contour, soft tissues can proliferate around it, and ridges will result trapped at the moment of testing the restorations.26
Pjetursson & al, support the idea that in a period of ten years, the cantilever survival estimated index is 81.5%. Success index lacking any complications is encouraging: 63%. An estimated 32.6% of all abutment teeth lost their vitality. > 9% of all teeth developed caries after 10 years.27
Current dental ceramic technology is advancing in leaps and bounds. New materials for tooth restoration are constantly produced. They have elicited great interest, since they offer aesthetic possibilities that are hard to achieve with ceramic-metal systems. Procera ® (Noble Biocare Inc) is an exclusively ceramic system in which computer-assisted design and manufacturing is used (CAD/CAM) to obtain a densely synthesized and extremely pure aluminum oxide coping. A scanner reads the stone-cement die in a specialized unit which processes data and creates a transverse bi-dimensional, or a tri-dimensional image on a computer screen. It allows for crown selection and modification before proceeding to the coping manufacture (CAD). This methods main advantage lies in the possibility of guaranteeing quality control through pre-established industrial criteria, during the process of coping re-manufacturing. This disposes of many operator-dependent variables which might have a bearing in coping manufacturing.
Marginal preparation might present a more chamfered design than a true shoulder. This is due to the greater resistance of this synthesized sub-structure.28,29
Aesthetic responsibility is not only circumscribed to shape, size and color of the tooth. An important fact is to preserve or recuperate dental-gingival harmony. Using any of the different alternatives offered by current materials, it is possible to attain perfectly adapted, very realistic resistant restorations. A comprehensive knowledge of these materials usage will allow the dentist to take maximum advantage of present dental technology to attain best possible results and provide optimal assistance to the patients.
CONCLUSION
Treatment success was based upon the following: maintaining stability of tissues surrounding the implant and periodontal tissues; periodontal architecture and masticatory function recovery, attainment of acceptable aesthetics results, and finally patient's functional and aesthetics satisfaction.
REFERENCES
1. Roblee RD. Interdisciplinary dentofacial therapy. A comprehensive approach to optimal patient care. Chicago, IL: Quintessence Publishing, 1994: 17-43. [ Links ]
2. Ibbetson R. Treatment planning. British Dental Journal 1999; 186 (11). [ Links ]
3. Jivraj S, Corrado P, Chee W. An interdisciplinary approach to treatment planning in implant dentistry. British Dental Journal 2007; 202 (1): 11-18. [ Links ]
4. Wikipedia: www.wikipedia.com.mx [ Links ]
5. Palazzo M, Massai L. The importance of the operating sequence: a multidisciplinary treatment approach. Pract Proced Aesthet Dent 2007; 19 (8): 483-9. [ Links ]
6. Roblee RD. Interdisciplinary dentofacial therapy. A comprehensive approach to optimal patient care. Chicago, IL: Quintessence Publishing, 1994: 17-43. [ Links ]
7. Meadows LM, Verdi AJ, Crabtree BF. Keeping up appearances: using qualitative research to enhance knowledge of dental practice. J Dent Educ 2003; 67: 981-90. [ Links ]
8. Lambert H. Accounting for EBM: Notions of evidence in medicine. Soc Sci Med 2006; 62: 2633-45. [ Links ]
9. Bader HI. Treatment planning for implants versus root canal therapy: a contemporary dilemma. Implant Dent 2002; 11: 217-23. [ Links ]
10. Dawson AS, Cardaci SC. Endodontics versus implantology: to extirpate or integrate? Aust Endod J 2006; 32: 57-63. [ Links ]
11. Doyle SL, Hodges JS, Pesun IJ, Baisden MK, Bowles WR. Factors affecting outcomes for single-tooth implants and endodontic restorations. J Endod 2007; 33: 399-402. [ Links ]
12. Salinas TJ, Eckert SE. In patients requiring single - tooth replacement, what are the outcomes of implant - as compared to tooth - supported restorations? Int J Oral Maxillofac Implants 2007; 22 (Supp l): 71-95. [ Links ]
13. Iqbal MK, Kim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int J Oral Maxillofac Implants 2007; 22 (Supp l): 96-116. [ Links ]
14. Clínicas odontológicas de Norteamérica. Endodoncia . Ed. Interamericana, 1984; 4: 917-921. [ Links ]
15. Shillinburg, Herbert T. Fundamentos esenciales de prótesis fija. 3a edición. Ed. Quintessence S.L., Barcelona, 2000. [ Links ]
16. Reeh, E, Messer H, Douglas W. Reduction in tooth stiffness as a results of endodontic and restorative procedures. J. Endod (1989), 15:512. [ Links ]
17. Steven A, Aquilino, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 2002; 87: 256-63. [ Links ]
18. Heling I, Gorfil C et al. Endodontic failure caused by inadequate restorative procedures: Review and treatment recommendations. J Prosthet Dent 2002; 87: 674-8. [ Links ]
19. Lui JL. Composite resin and reinforcement of flared canals using light-transmitting plastics posts. Quintessence Int 1994; 25: 313-319. [ Links ]
20. Thomas J. Salinas, DDS, Michael S. Block, DMD, and Avishai Sadan, DMD2004 American Association of Oral and Maxillofacial Surgeons Fixed Partial Denture or Single-Tooth Implant Restoration? Statistical Considerations for Sequencing and Treatment. J Oral Maxillofac Surg 62:2-16, 2004, Suppl 2. [ Links ]
21. Jones SD, Jones FR. Tissue-integrated implants for the partially edentulous patient. J Prosthet Dent 1988; 60: 349-54. [ Links ]
22. Blomberg S, Lindquist LW. Psychological reactions to edentulousness and treatment with jawbone-anchored bridges. Act Psychiatr Scand 1983; 68: 251-62. [ Links ]
23. Balshi TJ, Wolfinger GJ. Restoring lost vertical dimension of occlusion using dental implants: A clinical report. Int J Prosthodont 1996; 9: 473-8. [ Links ]
24. Henke DA, Fridrich TA, Aquilino SA. Occlusal rehabilitation of a patient with dentinogenesis imperfect: a clinical report. J Prosthet Dent 1999; 81: 503-6. [ Links ]
25. Kvist T, Reit C. The perceived benefit of endodontic retreatment. International Endodontic Journal 2002: 359-365. [ Links ]
26. Phuong D, Doan, Goldstein GR. The use of a diagnostic matrix in the management of the severely worn dentition. J Prosthodont 2007; 16: 277-281. [ Links ]
27. Pjetursson BE, Tan K, Lang NP, Bragger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. IV. Cantilever or extension FPDs. Clin Oral Implant Res 2004; 15: 625-642. [ Links ]
28. Marchack et al Customization of milled zirconia copings for all-ceramic crowns: A clinical report. J Prosthet Dent 2008; 99: 169-173. [ Links ]
29. May KB et al. Precision of fit: The procera allceram crowns. J Prosthet Dent 1998; 80: 394-404. [ Links ]
Note  Mailing Address:
Mailing Address:
Susana Mendoza Rivera
E-mail: susy.mrivera@gmail.com
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 texto en
texto en 


