1.Introduction
Radiation therapy over time has become an effective way to treat neoplastic diseases (cancer). High doses of ionizing radiation are imparted through radiotherapy to the tumor target tissue, protecting the surrounding risk organs. With the advance of technology, new techniques in radiotherapy have emerged: one of them is volumetric modulated arc radiotherapy (VMAT). With this technique, the radiation dose is administered with a high conformation and in shorter treatment times, compared to conventional radiotherapy techniques (intensity-modulated radiotherapy, IMRT). In VMAT, the administration of ionizing radiation to the patient is continuous, the gantry rotates in one or more arches, simultaneously varying three parameters: the dose rate, the gantry rotation speed and the opening of the multileafs 1. In the radiotherapy department of the National Institute of Neoplastic Diseases (Lima, Peru), there are approximately 15% of all new patients each year diagnosed with breast cancer; a certain number of patients receive VMAT treatments. While optimal dose distributions in VMAT are attributed to photon beam modulations, excessive modulation of a plan in VMAT (multiple parameters such as large number of MUs, complex- shaped segments, small apertures, and a large number of segments) can give a mismatch between planned and administered dose distributions to the patient 2. This is the importance of the verification of the dose distribution before the treatment, that is, the specific patient quality control; the most used method is through the analysis of the gamma index 3. For this, a treatment plan is carried out in a phantom (which is part of a verification system), with the same parameters with which the patient will be treated, subsequently, the phantom is irradiated, and the results of both dose distributions are compared, the calculated (by the treatment planning system, TPS) and the measured (by the verification system). The gamma index can be affected by both the precision of the TPS calculation and the precision of treatment delivery. For this reason, in this work the relative impact of parameters that influence the result of the gamma index for breast cancer treatments is evaluated and analyzed, and thus be able to apply it by establishing norms and/or criteria for evaluating the gamma index for the next patients, taking as reference the experience of the present study. In this way, a fundamental part of the Radiotherapy Quality Assurance Program will be fulfilled, the primary objective of which is to implement quality standards and criteria to ensure optimization of radiotherapy treatment and radiological protection of the patient.
1.1.Gamma index,
The gamma index, 𝛾, is one of the most used measures for the verification of techniques that use dose modulation, which compares the dose distribution measured in an array of detectors with the dose distribution calculated by the TPS. With current verification systems, three-dimensional dose distributions can be reconstructed from measurements of two-dimensional dose distributions and depth dose percentage (PDD) dosimetric data using a reconstruction algorithm. The gamma index combines the dose difference, ΔD, and the distance difference (distance to agreement, DTA), Δr. The dose difference is the percentage difference between the reference dose distribution (measured) and the evaluated dose distribution (calculated in the TPS). Because there may be high dose gradient regions, DTA is used. DTA is the distance between a measured point and the closest point in the dose distribution calculated with the same dose. In principle, both acceptance criteria were evaluated independently for regions of low and high dose gradient, but Low et al. introduced a method or formalism where they used both criteria, the dose difference and the DTA. This can be observed in Fig. 1. To calculate the γ, we first must find the minimum Euclidean distance for each reference point. Then, if the distance difference between the reference to the evaluated point is Δr(rR,rE), where rR is the reference point, and rE is the evaluated point, the dose difference, ΔD(rR,rE), is calculated using Eq.(1):
where DE(rE) is the dose at a point in the evaluated dose distribution, and DR (rR) is the dose at the reference point. Calculating the γ using Eq. (2), for each point in the evaluated distribution,
where δr is the distance difference criteria and δD is the dose difference criteria. The 𝛾 is taken as the minimum value calculated on all the evaluated points, see Eq.(3):
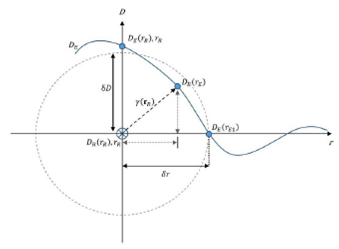
Figure 1 Schematic representation in one dimension of the gamma index. The y-axis is Dose, D, and the x-axis is distance, r. The intersection is the reference point, and the blue line represents the evaluated dose distribution 5.
The criteria δr and δD of an ellipsoid around the reference point as shown in 1. This method can be used as a pass-fail criterion, as :
Usually, γ is reported according to the criteria used, that is, δD(%)/δr(mm). The most widely used criteria for IMRT and VMAT treatments is 3%/3mm, which is the one originally recommended in Low et al. 4; however, this criterion may change according to the treatment area or the protocols established by the centers. During the analysis of γ, there will be points outside the field that will cause the result to decrease; so that these low doses do not influence the result, a lower dose threshold (LDT) is established, where 𝛾 is ignored. The AAPM in TG 119 recommends using an LDT of 10% 7; however, institutions based on their experience establish this value. In this work, we have used LDTs of 5% and 10%. Generally, the γ is calculated in two ways, local and global. For the local calculation, Eq.(1) and for the global calculation, we modify Eq.(1), so we have Eq.(5):
where Dnorm is a normalizing dose value, this can be the maximum dose from the reference dose distribution or a selected point on a high dose gradient. The local and global 𝛾 have advantages and disadvantages: the local tends to highlight failures in regions of high dose gradient, and in the global, these failures are less evident but show the errors within the high dose regions within the dose distributions. In general, the publications of the centers report the global index, but that will depend on what we want to analyze; for this, we have analyzed both forms of 𝛾 5.
2.Materials and methods
In order to carry out this work, the Linac Infinity (Elekta, Stockholm, Sweden) from INEN was used. This accelerator has 1 cm wide multileafs, projected in the isocenter. The materials and methodology developed in this work are described below.
2.1.Selection and generation of the treatment plan
For this work, 30 breast cancer treatment plans were evaluated, where both the breast and the supraclavicular region were treated at a prescribed dose of 5000 cGy in 25 fractions. These were planned in the TPS Monaco V.5.11.03 (Elekta, Stockholm, Sweden) with the VMAT technique and Monte Carlo calculation algorithm. The parameters used were semi-arches, with a calculation grid of 0.3 cm and an uncertainty of 1%. Each treatment plan was optimized to meet the tolerance dose constraints for healthy tissues established by the institution.
2.2.Octavius 4D system
For the specific patient quality control of each treatment plan, the Octavius 4D system (PTW, Freiburg, Germany) was used, which allows a volumetric gamma evaluation (3D), unlike its predecessors that allow doing a 2D gamma analysis of a single plane 8,9. This system has four basic components: motorized modular phantom, inclinometer, VeriSoft V7.1 software, and Octavius 729 detector array. The latter consists of a matrix of 729 air-vented cubic ionization chambers, the size of each chamber is 0.5 x 0.5 x 0.5 cm (0.125 cm3), with an effective measurement point located 0.75 cm below the matrix surface. The detectors are located at a distance of 1 cm between its centers and 0.5 cm between its edge, giving a total area of 27 x 27 cm. The detector array is placed inside the motorized modular phantom. This phantom is made of polystyrene with a density of 1.05 g/cm3 it is cylindrical with a diameter of 32.0 cm and a length of 34.3 cm. Both the detector array and the phantom rotate synchronously with the gantry (according to the angle measurement made by the inclinometer that is placed on the vertical part of the gantry) and measures the dose throughout the volume as a function of time and gantry angle (4D). In this way, the detector array always remains aligned perpendicular to the incident beam, measuring the dose plane for each gantry angle. The measurement data obtained is processed in the VeriSoft software, which having measurement data in 2D can reconstruct them in a 3D dose cube with a grid space of 2.5 mm 5. In this software, the measured dose is compared with the dose calculated in the TPS, in any particular plane or volumetric. The standard configuration of the Octavius 4D system in the treatment room is shown in Fig. 2.
2.3.Gamma index evaluation
For the evaluation of the gamma index, γ, the comparisons of the measured and calculated dose distributions were analyzed with the VeriSoft software, and different parameters were analyzed. One of these parameters is the normalization of the measured and calculated dose difference. There are two normalization methods, local (dose normalization at the corresponding position of the calculated matrix) and global (normalization in the maximum dose of the calculated dose distribution). Another parameter is the LDT, which is a percentage of the maximum calculated dose, which allows excluding points from the evaluation (possible measurements due to the effects of radiation scattering), which will not be considered in the analysis. A gamma passing rate, %GP, was defined as the percentage of points that satisfy the condition that the gamma index is lower than one 10. Works such as that of Heilemann et al.11 demonstrated that a global %GP of 90% with a criterion of 2%/2mm could detect clinically unacceptable VMAT plans. On the other hand, Hussein et al. and Fredh et al.12,13 showed that the %GP depends on the types of dosimeter used; likewise, the configuration and resolution of the detector have a great impact on the calculation of the gamma index pass rates. That is why in this work, we have considered different gamma analysis criteria, two types of normalization (global and local), and two LDT values mostly used in the institution and mostly reported in research papers. The summary of the parameters used for the gamma index analysis is shown in Table I.
3.Results
The results obtained are shown in of the 30 breast cancer treatment plans analyzed and using the gamma index analysis parameters of Table II.
Table II Mean gamma passing rate (%) with its respective standard deviation (σ).
| Analysis | LTD | Local gamma index | Global gamma index | ||
| criteria | mean | σ | mean | σ | |
| 1%/1mm | 5% | 36.3 | 2.8 | 61.9 | 4.0 |
| 10% | 37.9 | 3.0 | 55.9 | 4.1 | |
| 2%/2mm | 5% | 67.0 | 3.7 | 87.4 | 2.6 |
| 10% | 69.2 | 3.8 | 84.8 | 3.1 | |
| 2%/3mm | 5% | 83.9 | 2.8 | 94.2 | 1.5 |
| 10% | 86.6 | 2.6 | 93.0 | 1.9 | |
| 3%/2mm | 5% | 70.5 | 3.9 | 92.2 | 2.1 |
| 10% | 72.8 | 3.9 | 90.3 | 2.7 | |
| 3%/3mm | 5% | 85.8 | 2.8 | 96.5 | 1.2 |
| 10% | 87.6 | 2.6 | 95.6 | 1.6 | |
| 3%/3mm | 5% | 89.3 | 2.6 | 98.7 | 0.7 |
| 10% | 91.1 | 2.3 | 98.4 | 1.0 | |
Regarding the analysis of the local gamma index, from Fig. 3, it can be observed that the mean %GP increases to 2.3% at the LDT of 10%, compared with that of 5% for the criterion of 3%/2 mm and increases 1.5% for 1%/1 mm (Fig.3a)). The opposite happens in the analysis of the global gamma index, where a decrease in the mean of the %GP of up to 6% is seen for the LDT of 10% compared to that of 5% for the criteria of 1%/1 mm, and a decrease of 0.3% for 5%/3 mm. This difference from the average %GP is more noticeable in stricter gamma index criteria such as 1%/1 mm and 2%/2 mm (Fig.3b)). These results agree with the work carried out by Song et al. 10, where the increasing trend of %GP for LDT from 0% to 15% was up to 10.16% for local gamma index analysis and a decreasing trend of %GP from LDT of 0% to 15% was up to 0.23% in the global gamma index analysis in brain treatments for analysis criteria of 3%/3 mm. For all cases of breast cancer in the local gamma index analysis for criteria of 3%/3 mm and 5%/3 mm, the results of the mean %GP are between 85.8% (LDT of 5%, criteria of 3%/3 mm) and 91.1% (LDT of 10%, criteria of 5%/3 mm). With these same criteria for the global gamma index analysis with the LDT of 5% and 10%, they had a %GP above 95%, as shown in Fig. 3(c and d).
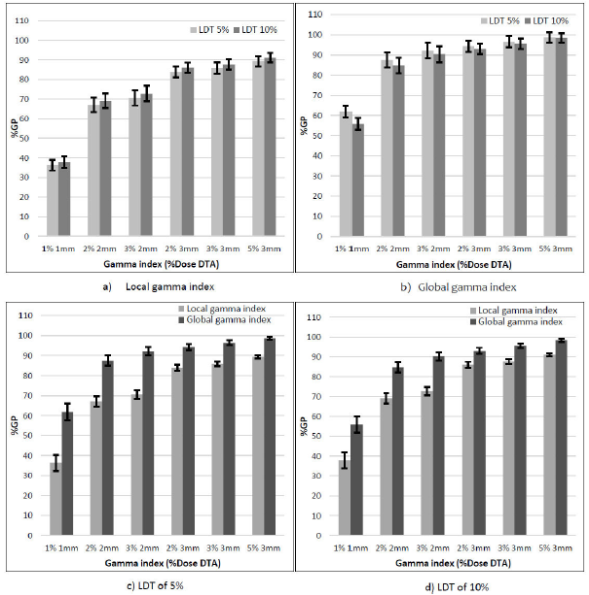
Figure 3 %GP for different analysis criteria. a) Local gamma index, b) Global gamma index, c) LDT of 5% and d) LDT of 10%.
Likewise, a difference of 25.5% is seen between the global and local index for criteria of 1%/1 mm at LDT of 5%; this difference decreases to 18.0% for the LDT of 10%. As the criteria are not as stringent, this difference decreases, 9.4% (LDT of 5%) and 7.3% (LDT of 10%) for the 5%/3 mm criteria. The differences found in the behavior of the local and global gamma index shown in this study coincide with the reports by Yu L. et al. and Stasi M. et al. 14,15, which report that the two forms of normalization exhibit specific and sensitive variations to dose administration errors.
It can be seen from Fig. 4 that the standard deviation is lower in the global gamma index analysis than in the local, and this variation explains as the analysis criteria are less strict. Likewise, in the global gamma index analysis, it is observed that the standard deviation is slightly lower at the LDT of 5% compared to that of 10%.
4.Conclusions
From the parameters analyzed for the analysis of the gamma index (normalization, analysis criteria, LDT), it is concluded that the mean of %GP of the global gamma index is greater than the mean of %GP of the local gamma index when using the same analysis criteria and LDT; and that is typical of normalization in each analysis, in the global gamma, the percentage differences of each point are normalized to the maximum planned dose, while in the local gamma the percentage differences of each point are normalized to the expected dose at that point. In addition, it is concluded that the mean %GP decreases in the analysis of the global gamma index and increases in the local gamma index if we compare the LDT from 5% to 10%. However, these differences are not of great impact on the analysis. Likewise, the standard deviation is less for the LDT of 5% compared to that of 10%; for the analysis of the global gamma index, this decrease in standard deviation is more noticeable while the analysis criteria are not so strict (5%/3 mm). We recommend that each local and global gamma index analysis should be used carefully since neither can substitute for the other and while dose differences could be overestimated in local gamma index analysis, global gamma index analysis could underestimate these dose differences in low dose regions. However, the global gamma index analysis will show the errors of the higher dose regions, as opposed to the local gamma index, which does not highlight these errors. The choice of parameters and the type of analysis to be used will depend on the quality control test to be performed.











 nueva página del texto (beta)
nueva página del texto (beta)




