Introduction
Neurodegenerative diseases (ND) are a set of central nervous system conditions whose main characteristic is the appearance of progressive damage that affects cognitive and motor functions. These diseases are usually of sudden onset, and there are no specific treatments to reverse or stop their progression; therefore, the patient’s fate is death1.
There are four NDs with the highest prevalence worldwide: Alzheimer’s disease (AD), in the first place, is the leading dementia affecting 15/1000 people; Huntington’s disease is a motor disease that afflicts 12/100000 people; and Parkinson’s disease (PD) occurs in 5 out of 100000; whereas Amyotrophic Lateral Sclerosis (ALS) prevalence is 1.75-3/1000002,3.
These diseases burden health systems worldwide because they are disabling and significantly deteriorate people’s life quality and expectancy. In addition, there is a negative impact on the family life of affected people related to the high costs of the necessary care and treatment.
Although there are numerous theories about the origin of these ND, there is a lack of precision in pointing out the causes of these diseases, which results in the absence of etiological treatments; for that reason, therapies are usually only palliative4. A probable cause is the alteration in mitochondrial function or mitochondrial dysfunction, which is widely studied.
Mitochondria play fundamental roles in the central nervous system, that is, as a supplier of energy that cells need to fulfill their functions; therefore, the organelle’s function must be kept in optimal condition because they are the cellular site for cellular ATP synthesis. Other main mitochondria functions are the regulation of intracellular calcium concentrations, functioning as transitory calcium stores and as a regulator and amplifier for intrinsic apoptosis, being a center where different intracellular routes converge, and, in addition, mitochondria participate in the synthesis of some steroids and neurotransmitters5.
In recent years, several reports have described severe alterations in different mitochondrial functions associated with primary ND (Table 1); however, it is still unclear whether mitochondrial dysfunction is a cause or one consequence of other pathological mechanisms existing in the evolution of these diseases.
Table 1 Main mitochondrial alterations associated to clinical manifestations in patients with neurodegenerative diseases
| Pathology | Clinical manifestation | Impaired structures | Mitochondrial disorder | References |
|---|---|---|---|---|
| Alzheimer | –Episodic and spatial memory loss – Learning difficulty – Language loss |
– Hippocampus | – Altered mitochondrial dynamics – Oxidative stress – Impaired apoptosis – Calcium imbalance |
Manczak et al. 2018 Reddy et al. 2018 Erickson et al. 2012 |
| Parkinson | – Tremors – Parkinsonian gait – Hypogenesis – Dementia |
– Dopaminergic system – Locus niger |
– Altered mitochondrial dynamics – Oxidative stress – Impaired apoptosis |
Borsche et al. 2021 Rao et al. 2014 Lin and Beal, 2006 |
| Huntington | – Motor deficit – Lack of emotion recognition – Lower processing speed – Visuospatial problems |
– Cerebral cortex – Hippocampus – Hypothalamus – Striatum – Putamen |
– Altered mitochondrial dynamics – Oxidative stress – Impaired apoptosis |
Naia et al. 2016 Costa et al. 2010 Benchoua et al. 2006 |
| Lateral amyotrophic sclerosis | – Progressive motor deficit – Dementia in 5-15% of cases |
– Brainstem – Spinal cord |
– Oxidative stress – Impaired apoptosis |
D’ Amico et al. 2013 Simpson et al. 2004 Wiedemann et al. 2002 |
Roles of mitochondria in health and disease
Mitochondrial ATP is synthesized through a mechanism known as oxidative phosphorylation carried out in the inner membrane by a serial group of five protein complexes named Electron Transport Chain (ETC) (ETC, Fig. 1). The ETC generates an electrochemical gradient by pumping protons from the mitochondrial matrix to the intermembrane space, using a flow of electrons between complexes I, II, III, and IV as an energy source. Finally, electrons are used to reduce oxygen to water. In contrast, the force generated by the proton gradient is used by ATP synthase to convert ADP and inorganic phosphate to ATP (the proton-motive force)6.
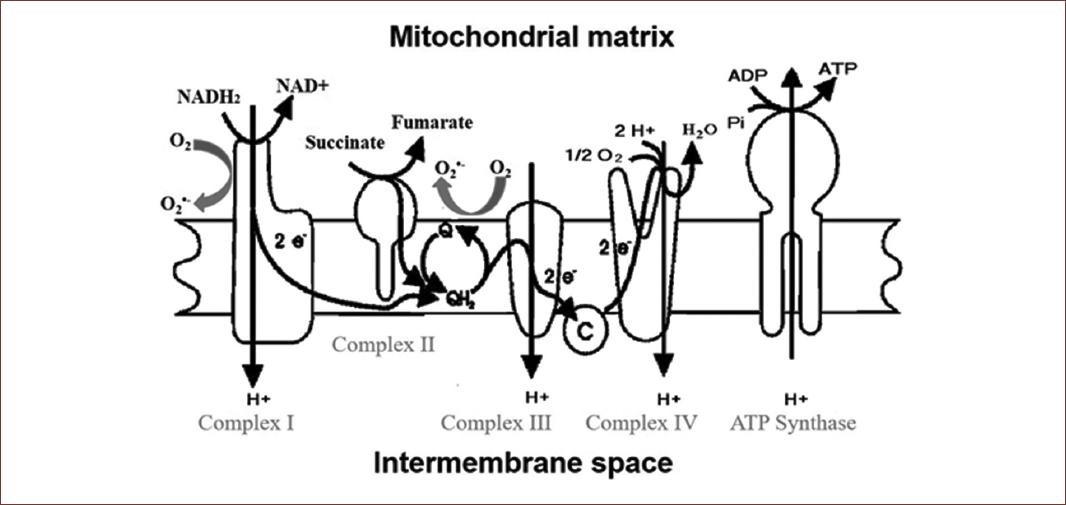
Figure 1 Schematic representation of the electrons flow through the mitochondrial electron transport chain, the translocation of protons by complexes I, III, and IV, and the synthesis of ATP by ATP synthase from ADP and phosphate; additionally, the figure shows the sites identified as the source of superoxide radicals: Complex I and Q-cycle. It was modified from Martinez-Abundis et al. 2005.
On the other hand, the mitochondria are the organelle where more free radicals are produced. In the processes of oxidative phosphorylation, oxygen is reduced to water by accepting two electrons. Still, this reduction can be incomplete and generate the radical superoxide in mitochondrial Complex I and IV of the ETC as an undesirable product of the ATP synthesis (Fig. 1). Under normal conditions, free radicals are produced in small amounts that either comply with physiological functions or are counteracted by an antioxidant system conformed by both enzymatic (superoxide dismutase, glutathione peroxidase, and catalase), and non-enzymatic compounds, such as ascorbic acid or Vitamin E7,8.
Under pathological conditions, damage to its components or overload in the ETC may favor the overproduction of reactive oxygen species (ROS) or free radicals. In general, up to 2% of oxygen consumed by the ETC is partially reduced to superoxide but may increase significantly, forming another ROS like oxygen peroxide (Fig. 2). In the development and evolution of main ND, environments of high oxidative stress are generated9.
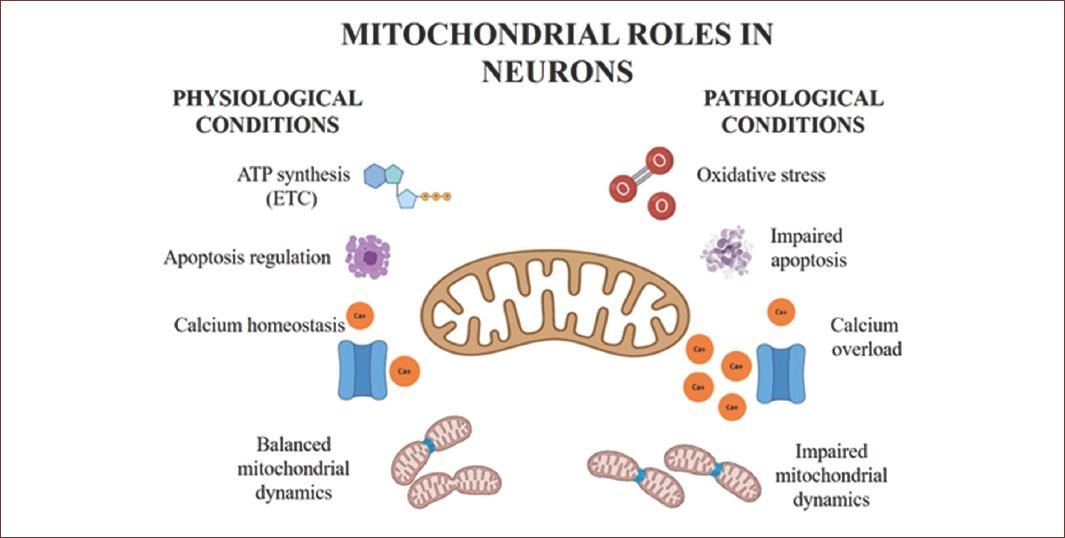
Figure 2 Schema shows the functions and events that occur in the mitochondria. On the left are the physiological processes in healthy neurons and on the right are the conditions in different pathological states associated with neurodegenerative diseases. ETC: Electron Transport Chain.
Mitochondria, contrasting with other organelles, cannot be generated de novo; therefore, they must be renewed from pre-existing mitochondria. This process, called mitochondrial dynamics, consists of two mechanisms: In mitochondrial fusion, two mitochondria come together to form one, to exchange their content and thereby alleviate defects such as genetic mutations or functional damage in proteins resulting from the free radicals production10. The second process is fission when one mitochondrion divides in a controlled manner to generate two smaller organelles. Fission is necessary for generating a higher mitochondrial population and may respond to an increased necessity of energy, or like fusion; it represents a way to deal with damaged mitochondria since smaller defective mitochondria may be eliminated by mitophagy. Mitochondrial dynamics are vital for neurons since the energy demand to carry out their functions is very high. These organelles’ cellular distribution impacts neuronal function, so even a tiny imbalance could be catastrophic for these cells.
Mitochondria regulate the intrinsic pathway of apoptosis, serving as a reservoir for some pro-apoptotic factors such as cytochrome c, which, once released to the cytosol, binds to the adapter protein Apaf 1 and procaspase 9 to assemble the apoptosome. This complex’ function favors the caspase 9 self-activation and amplifies the apoptotic signaling to cell death11. The extrinsic pathway, not dependent on mitochondria, begins with the activation of death receptors, including TNF type 1 and Fas, by external stimuli and ends with the activation of effector caspases12. The intrinsic and extrinsic pathways may converge because caspase 8 activates Bid, a pro-apoptotic protein that further will translocate from the cytosol to the outer membrane of the mitochondria, increasing its permeability and allowing the release of cytochrome C13. Intrinsic apoptosis is tightly regulated through different mechanisms, for example, the Bcl-2 family of proteins (Bcl from B-cell Lymphoma) integrated by both pro- and anti-apoptotic members. Pro-apoptotic proteins such as Bad, Bid, and Bax promote the permeabilization of the outer mitochondrial membrane, whereas Bcl-2, Bcl-XL, among others, counteract these effects by acting as anti-apoptotic factors.
The opening of the mitochondrial permeability transition pore (mPTP), an unspecific transmembrane channel in the inner membrane that, once opens, allows the crossing of solutes, is another possible route for activating the intrinsic pathway of apoptosis. The mPTP is a channel whose structural identity is still under discussion; however, a hypothesis suggests it is integrated at least by three proteins: the constitutive outer membrane voltage-dependent anion channel, the inner membrane adenine nucleotide translocator and the isomerase cyclophilin D, located in the mitochondrial matrix. This pore is formed to regulate the mitochondrial excess of calcium. Still, some stimuli, such as the increase in ROS or a calcium overload, induce a more extended opening, causing mitochondrial swelling, a massive entrance of water, and the leakage of cytochrome c to the cytosol14.
Intracellular calcium levels play a fundamental role in neurons’ functions, but high concentrations may disturb the bioenergetics and functionality of the mitochondria. The largest intracellular calcium reservoir is the endoplasmic reticulum; however, the mitochondria may contain it temporarily when a massive release to the cytosol. If the calcium overload is persistent, a collapse in the membrane potential, ATP depletion, and the generation of ROS will promote the activation of cell death15.
The proper function of mitochondria depends on two crucial processes: Biogenesis and mitophagy. The first comprises the formation and growth of new mitochondria from pre-existing ones, the mechanism described previously as mitochondrial dynamics. The whole process includes the replication of mitochondrial deoxyribonucleic acid (DNA), the synthesis of membranes’ components, and the synthesis and importation of proteins encoded by both the mitochondrial and nuclear genomes. For the successful occurrence of these processes, tight coordination between the processing of both genomes (nuclear DNA codifies for most of the mitochondrial proteins, whereas mitochondrial DNA only codifies for a small number) is required.
Mitochondrial biogenesis is regulated mainly by Peroxisome proliferator-activated receptor gamma 1-alpha coactivator (PGC-1α), among the nuclear respiratory cofactors 1 and 2 as well as receptors activated by peroxisome proliferators gamma16. On the other hand, mitophagy is the specific process for eliminating damaged mitochondria, being the only way to remove these organelles. The whole process is regulated mainly by two proteins, Protein Kinase 1 and Parkin, which first accumulate in the membrane of damaged mitochondria to promote their separation from the mitochondrial network, subsequent ubiquitination, and finally, their degradation17.
Alzheimer
Alois Alzheimer first described AD. It is one of the most relevant ND and the most frequent form of dementia; additionally, it is an age-specific disease mainly affecting people over 60 years18.
The gradual, progressive, and irreversible loss of cognitive abilities, such as spatial memory, working memory, and motor coordination, characterize AD. Although its origin is still unknown, the main pathophysiological characteristics of the disease are well identified: (1) the hyperphosphorylation of the TAU protein, a cytoskeleton stabilizer, induces its dissociation and tends to form aggregates called neurofibrillary tangles, which alter entirely the cellular structure, inducing its death; (2) the β-amyloid peptide is over-produced and tends to forms the neurotoxic aggregates called amyloid plaques, which alter the cellular structure and function. These changes usually start in the hippocampus; however, in advanced stages of AD, they may extend to the cerebral cortex19.
Regarding mitochondrial functions, the interaction between the β-amyloid peptide and its protein precursor with mitochondria was described within the molecular alterations of AD, altering its normal functioning and making this a preponderant damaging event in neurodegeneration20. The mitochondrial fission-associated protein Drp-1 is activated by nitrosylation in the hippocampus and cerebral cortex of genetically modified mouse models whose overexpression generates its accumulation. The expression of Fis-1, another fission-associated protein, is also increased. These changes also explain another pathological finding, the increased number of smaller mitochondria. In addition, the down-regulation of fusion proteins OPA 1 and mitofusin 1 and 2 was observed, rendering a lower rate of mitochondrial fusion and an imbalance toward fission. As fission is a vital process for the recycling of mitochondrial components, its stimulation can be interpreted as an indicator of the poor health of these organelles21 and the fact that increased fission is associated with the accidental release of cytochrome C and the activation of apoptosis.
In mouse hippocampal neurons treated with β-amyloid peptide, considered an in vitro model to study the pathogenesis related to the development of AD, mitochondrial fission was upregulated, and fusion downregulated in addition to alterations in both biogenesis and mitophagy. In addition, oxidative stress increases considerably due to the treatment22.
According to the previous reports, once in the cytosol, the β-amyloid peptide is internalized into the mitochondria through inner and outer membrane-located translocases23, which may interfere with the importation of nuclear-encoded ETC subunits, affecting assembly or function of the mitochondrial complex. There is experimental evidence of impaired functioning of complexes I (NADH dehydrogenase), III (Cytochrome C Reductase), and IV (Cytochrome C Oxidase) as a result of β-amyloid peptide interaction. This effect modifies the oxidative phosphorylation (electron flow, the proton gradient, and mitochondrial potential), which finally will affect the synthesis of ATP by complex V (ATP synthase)24 and increase the formation of ROS as sub-products (Fig. 2).
The triggering of oxidative stress by β-amyloid peptide has different consequences on the central nervous system cells; for example, it increases lipid peroxidation, affecting mainly the polyunsaturated fatty acids, constituents of biological membranes, which turned into loss of membranes fluidity, modification of the membrane potential and increased permeability. Proteins undergo oxidative damage, such as carbonylation and nitrosylation, which modify their structure and compromise their functionality. Increased oxidative stress may also induce mitochondrial and nuclear DNA mutations, affecting the proteins’ expression and function25.
The tight regulation of calcium concentrations is essential for the properly functioning of the central nervous system. In this sense, the previous reports indicate that calcium homeostasis is altered in AD, probably because mitochondrial dysfunction decreases its capacity to absorb and retain calcium, specifically in the case of mitochondria located at the synaptic button. These disturbances in calcium management produce defects in the release of neurotransmitter-carrying vesicles. In addition, the endoplasmic reticulum releases stored calcium, increasing its cytosolic concentration and promoting the opening of pores in the mitochondrial membrane that allow the releasing of pro-apoptotic factors, including cytochrome C, which finally activate the intrinsic pathway of apoptosis26. The decreased size of structures such as the hippocampus and cerebral cortex that characterizes AD is associated with increased apoptotic cell death, which is recognized as the leading cause of the decline in cognitive abilities that characterize this disease27.
There are additional mechanisms reported for mitochondrial damage; for example, aging is associated with structural and functional changes, including a decrease in the number of inner membrane cristae, the dissociation of ATP synthetase dimers, and the accumulation of mutations in mitochondrial DNA, which culminates in metabolic alterations, accompanied by an environment of high oxidative stress and apoptosis which finally is potentiated by the characteristic accumulation of β-amyloid.
Genetics could be a central pathological component contributing to the transition from mitochondrial failures to dysfunction. The mitochondrial DNA is highly susceptible to mutations induced by the oxidative stress generated by the organelle, which, added to the lack of histone protection, may accentuate the failures in energy metabolism since the mitochondrial genome codifies for numerous subunits of protein complexes of the respiratory chain.
Similarly, lifestyle and environment may increase the risk of developing AD. Exposure to toxins such as pesticides, xenobiotics, and heavy metals induces neurotoxicity and mitochondrial dysfunction, which causes symptoms similar to those of Alzheimer´s disease. On the other hand, the consumption of hypercaloric diets is associated with a deficit in mitochondrial functioning due to an increased generation of oxidative stress28.
The mitochondrial defects mentioned above modify the energy metabolism; therefore, positron emission tomography and fluorodeoxyglucose (FDG-PET) can be used for the diagnosis of the disease because the detection of a lower uptake of cerebral glucose is possible with this technique and may be related to cognitive symptoms in patients with the presence of Alzheimer disease29.
PD
PD was described by James Parkinson in 1817 and called palsy agitans2. It is a progressive neurological disorder that courses with motor symptoms such as bradykinesia (slowness of movement), stiffness, or involuntary resistance to movement, besides tremors at rest and postural instability due to the difficulty in maintaining or changing postures while walking or walking stand. Non-motor and psychiatric symptoms may also occur as loss of smell, difficulty sleeping, REM sleep disorders, constipation, urinary frequency, erectile dysfunction, orthostatic hypotension, and changes in blood pressure. In addition, symptoms such as anxiety, depression, psychosis, apathy, and dementia are added30.
The neuropathology of PD involves mainly the deregulation of dopaminergic neurotransmission, degeneration of nerve fibers, and neuronal death due to α-synuclein deposits forming structures known as Lewy bodies. The affected structures in the central nervous system are the cerebral cortex, the brain stem, the spinal cord, the hypothalamus, and the insula. In contrast, at the peripheral level, the enteric neural plexus and the vagus nerve are affected31.
According to reports, the mitochondrial damage in PD is extensive. The protein α-synuclein accumulates inside the mitochondria of people’s brains, interfering with the ETC by decreasing the activity of complex I (NADH dehydrogenated) and simultaneously increasing oxidative stress by overproduction of ROS32.
Results from experimental models indicate that blocking complex I of the ETC induces dysfunction in dopaminergic neurotransmission33; the main transmission route affected in Parkinson’s disease is the substantia nigra, which initially decreases the complex I activity. In addition, reports indicate that mitochondrial complex I subunits are oxidized, and activity is reduced in multiple tissues from individuals with sporadic PD, probably associated with incorrect assembly and anchoring of complex I to the inner mitochondrial membrane34. These effects are associated with an increase in the mitochondrial permeability transition, which raises the generation of ROS and, therefore, a state of oxidative stress in the central nervous system35.
Mitochondrial dysfunction may also result from defects in biogenesis, as suggested by the analysis of the substantia nigra samples obtained from autopsies of patients with PD, where the coactivator of transcription factors PGC-1α expression was downregulated36; such a result correlated with the increased expression and oligomerization of α-synuclein37. On the other hand, an increased expression of Pink and Park, the main proteins involved in mitophagy regulation, suggests this process is also affected9.
There are rare, autosomal, and dominant forms of the disease that include mutations in the PINK1 (PTEN-induced kinase 1) and PARKIN (ubiquitin ligase) genes, which were described as causing a pathology very similar to sporadic PD; however, they could be considered more a type of parkinsonism than the true disease whose primary etiological agent is accumulations of α-synuclein38.
These genes control the elimination of defective mitochondria, adjusting the mitochondrial network and thus maintaining the homeostasis of energy metabolism. PINK1 regulates the translocation of PARKIN in damaged mitochondria and promotes its elimination through a type of selective autophagy (mitophagy); as these genes are mutated and the consequent defective production of these proteins, as well as the lack of expression of the same, they interrupt the signaling for the initiation of mitophagy, therefore, there is an accumulation of damaged mitochondria, and accumulation of more failures in energy metabolism39.
Huntington disease
It is an autosomal dominant disease, described first by George Huntington in 1872, who discovered its hereditary nature. Huntington’s disease (HD) is a motor disorder such as chorea (involuntary and irregular movements of extremities) and loss of coordination, with the appearance of psychiatric symptoms such as depression, psychosis, and obsessive-compulsive disorder. The brain structures damaged in this disease are the caudate nucleus and the putamen; both are part of the striatum. In addition, there is a loss of spinous efferent neurons and a thinning of the cerebral cortex, which occurs at the early stages of the disease and may explain its heterogeneity40.
The HD-associated disturbs result from mutations in the gene that codes for Huntingtin. This 350 kDa protein contains uninterrupted repeats of CAG triplets in its first exon. While the normal allele includes a maximum of 35 repetitions, the mutant allele contains 36 or more. Significant findings are that only a small number of patients with 36-41 repeats have symptoms and that at a higher number of repetitions, the age for the onset of symptoms is lower41.
Postmortem studies carried out either in the brains of patients with HD or in experimental models showed a dramatic decrease in the activity of mitochondrial complexes II, III, and IV in both the caudate nucleus and putamen42,43 which is associated with low ATP levels, increased oxidative stress and cell dysfunction44 These disturbances may result from a decrease in glucose metabolism since alterations in the function of the enzyme glyceraldehyde 3-phosphate dehydrogenase were detected (GAPDH)45.
On the other hand, mitochondria’s morphology is abnormal due to an imbalance between fusion and fission, assessed as an increased expression in the fission-related proteins Drp-1 and Fis-1, besides a decrease in the fusion-related proteins, mitofusins, and OPA-1 (Fig. 2). As described above, this modification in either the brains of patients with the disease or in experimental models leads to excessive mitochondria fragmentation46.
ALS
It is a progressive motor disease described by the French physician Jean-Martin Charcot in 1869. The main feature of this disease is the degeneration of both the upper motor neurons that connects the cortex with the brainstem and spinal cord, as well as the lower motor neurons that link the brainstem and spinal cord with the muscle; that is why the symptoms are usually motor and extra-motor47. Signs that progress over weeks or months include dysarthria, slurred speech, spasticity or muscle stiffness, dysphagia or difficulty swallowing, and muscle weakness. Unlike other motor diseases, such as PD or Huntington’s chorea, psychiatric symptoms do not manifest in ALS. Patients suffering from this disease and their families may improve their quality of life with palliative and supportive therapies.
The pathophysiology of ALS is partially unknown; however, aggregates of a protein called TDP-43 were identified in people with this disease. This protein is encoded in the TARDBP gene, and the formation of aggregates is associated with the misfolding induced by genetic mutations48. Like the other ND, mitochondria may be one of the most affected organelles since ATP generation is decreased, possibly due to reduced activity of complexes I, II, III, and IV49,50. In addition, there is an increase in the production of ROS, oxidative stress51, and, finally, a high rate of lipid peroxidation52.
Alteration in genes involved in mitochondrial function and homeostasis have been described in patients and mouse models with the disease; for example, mutations in the antioxidant enzyme Superoxide dismutase 1 gene, which has cytosolic and mitochondrial isoforms, favors the formation of mitochondrial aggregates, inhibiting respiration53. On the other hand, the gene that encodes the C9ORF72 protein suffers mutations in ALS, which trigger the formation of toxic mitochondrial aggregates, and increases the mitochondrial membrane potential along with the formation of ROS. In addition, this protein participates in the assembly of Complex I and interacts with the ATP5A subunit of Complex V; hence, its mutations may translate into a dysfunctional Complex I and a decrease in ATP production, respectively.
It has been reported that the gene that encodes the RNA- binding protein FUS (FUS) is altered at the early stages of ALS. This protein is responsible for directing the mRNA encoding the respiratory chain proteins, which hinders their expression with consequences such as disruption of the mitochondrial network, decreased oxygen consumption, and increased ROS production.
Mutations in the gene that encodes the Vesicle-associated membrane protein B that participates in the transfer of lipids, as well as calcium ions, have diverse effects on mitochondrial function as a lower importation of calcium from the endoplasmic reticulum to mitochondria, reduction in the activity of the respiratory chain and, it has also been associated with defective autophagy.
Similarly, mutations in other genes responsible for mitochondrial quality control and mitophagy, such as Valolin-containing protein, Optineurin, and TANK-binding kinase 1, which hinders proper mitochondrial transport and recycling, were described. Mutations in the SIGMAR1 gene that encodes the Sigma 1 opioid receptor induce a rupture of mitochondrial membranes, resulting in a loss of membrane potential and a decreased ATP production.
Finally, the gene for the Kinesin family member 5, a protein that participates in the transport of organelles, including mitochondria, is affected, resulting in its incorrect distribution through the neuron53.
Conclusion
Mitochondrial dysfunction is a common characteristic in the main ND, which is unsurprising, considering its relevance for the ATP supply to cells. The energy supply to neurons is compromised under pathophysiological environments, with a collapse in ATP production and an increase in ROS generation; both are commonly found and, even more, may be considered markers for the pathophysiology of ND. In addition, some mitochondrial mechanisms, such as fission and fusion, biogenesis, and mitophagy, which participate in the recycling and maintenance of the organelle are often affected. Neurons’ functionality depends on a strictly controlled environment; these changes can ultimately lead cells to apoptotic death and neurodegeneration (Fig. 2). Nowadays, the evidence of mitochondrial alterations’ participation in ND is abundant; the evidence also indicates that preventing mitochondrial dysfunction may diminish or stop the progression of neurological damage, placing mitochondrial dysfunction as an essential part of the disease process over a single consequence.











 nueva página del texto (beta)
nueva página del texto (beta)


