Introduction
In Mexico, Type 2 Diabetes Mellitus (T2DM) is considered a public health problem (American Diabetes Association, ADA, 2019, 51). Data from the National Health and Nutrition Survey, Medio Camino (Instituto Nacional de Salud Pública, INSP, 2016, 46), show that T2DM constitutes 92-95% of cases diagnosed with the disease. The prevalence of T2DM in adults between 50 and 80 years old, is around 24%, with a maximum peak in the generation of the sixties that corresponds to 30.3%. This anticipates a scenario with a greater number of adults suffering from chronic degenerative diseases, where T2DM and complications derived from it stand out, which negatively impact the state of health and well-being of adults of older age, whose demography grows exponentially in the country (Consejo Nacional de Población, CONAPO, 2017, 3). These facts lead to important considerations in two senses: intensify preventive measures that decrease the incidence of T2DM, and look for strategies to prevent complications in older adults already diagnosed; for this it is necessary to identify casual factors or associated to the two states mentioned above.
Despite of an increase in the efforts of preventive programs by the health sector, the trend of T2DM in the last decades has increased 2.7% every year in Mexico (Rojas-Martínez, Basto-Abreu, Aguilar-Salinas, Zárate-Rojas, Villalpando, Barrientos-Gutiérrez, 2018, 224). Despite the fact that people living in larger localities have greater access to health services, the prevalence of T2DM is greater in urban areas compared to rural areas (Rojas-Martínez et al., 2018, 224; INSP, 2012, 22).
During the last decades, several factors are related to T2DM, highlighting the genetic or family antecedents, high body mass index, obesity, arterial hypertension (Cederburg, Stancakova, Kuu-sisto, Laakso, Smith, 2015, 540). In order to obtain a better explanation in the increase of cases of T2DM in the population, psycho-social and economic variables such as health perception, social support, stress, depression, education level, the social stratum, and the economic income have recently emerged as risk factors (Adler and Stead, 2015, 373). In this sense, the term "social determinants of health" allows to extend the explanatory-causal horizon, towards social/community institutions and policies involved with the provision of health services to citizens, that include factors that determine living and working conditions of the population, a vision that has been established as the basis for the Socio Ecological Model (Bravemant and Gottlieb, 2014, 20).
The Socio Ecological Model postulates that factors of an intrapersonal, interpersonal, organizational, community type and derived from public policy; factors influencing individual level in health-disease situations. These are organized in concentric strata, which interact with each other, around the individual impacting health directly and indirectly (Krieger, 2001, 669; Sallis, Owen, Fisher, 2008, 470). This model focuses on the individual, immediate, and mediate environmental factors that influence their health status, constituting an appropriate framework to identify and understand the synergy of variables of different origin, and level of influence in the development of T2DM, and its complications (Hill et al., 2013, 2434). In this context, people older than 50 years often face an important allostatic overload caused by the normal aging process, which can be aggravated by the appearance of environmental factors that favor the development of diseases such as T2DM (Riveiro, Amaro, Lisi, Fraga, 2018, 1092).
It is essential to identify causal or associated factors of the "diabetes epidemic" in the country, to promote programs and strategies that contribute to the reduction of the problem, currently described as "critical", since the family and government impact is such, that of maintaining the current trend, resources will be insufficient both for the health sector and for families (Barraza-Lloréns et al., 2015, 15). The literature reports a series of interventions "successful" programs focused on modifying behaviors of the individual with T2DM or at risk of suffering it (Huang, Pan, Chen, Chen, Chen, Hu, 2016, 47). Unfortunately, these have not impacted the trends in the country where the incidence and prevalence of T2DM continues to rise (Rojas-Martínez et al., 2018, 230). The identification of the influence of individual and environmental factors, up to where it was investigated, it has not yet been done in national representative samples.
In the context of the socio-ecological model, the present investigation posed the question: What individual and environmental factors explain the presence of T2DM in a representative sample of the adult population of Mexico?
Data
The data for this study come from the Mexican Health and Aging Study (MHAS) (National Institute on Aging, 2015). The MHAS is a nationally representative longitudinal survey of adults 50 years and older, it is collected by the National Institute of Geography and Statistics in collaboration with Universities of Pennsylvania, Maryland, Texas Medical Branch, and Wisconsin, the National Institute of Public Health and the National Institute on Aging. The objective of the survey is to collect information regarding Mexican adults’ aging process, diseases, individual behaviors, migration, community and households characteristics, and explore intergenerational changes in health conditions. The MHAS consists of four phases: 2001, 2003, 2011, and 2015. For this study we used information from 2015.
The target population of this study is comprised of men and women older than 50 years old residing in rural and urban areas of Mexico. The dataset contains 14,351 cases. The data were screened for missing values and outliers. Missing values and outliers represent 8.13% of the dataset. We used listwise deletion to deal with missing values and outliers. The final dataset resulted in a sample size of 13,186 valid cases.
Variables
Diabetes. The outcome variable of this study consists of a dichotomous variable that indicates 1 if the respondent has been ever been diagnosed by a physician or medical personnel with diabetes, and 0 otherwise.
Health perception. This variable is indicated by respondents’ health perception. The respondent was asked how they consider their health conditions. Responses were coded as 1 poor, 2 fair, 3 good, 4 very good, and 5 excellent.
Depression. This is a dichotomous variable indicating 1 if during the last two years the respondent has ever felt sad, blue, or depressed for more than two weeks in a row, and 0 otherwise.
Exercise. This variable aims to measure respondents’ exercise habits. Respondents were asked if, in average, they have exercised or done hard physical work three or more times per week in a row during the last two years.
Sleep problems. This variable is a composite scale estimated from five questions: I) how often do you have trouble falling asleep?; II) how often do you have trouble with waking up during the night (after you have been falling asleep)?; III) how often do you have trouble with waking up too early and not being able to fall asleep again?; IV) how often do you feel really rested when you wake up in the morning? Responses of each question, except question four, were coded as 3 indicating most of the time, 2 sometimes, and 1 never or rarely. Responses of question four were coded as 3 indicating never or rarely, 2 sometimes, and 1 most of the time. Responses of the four questions were added to create a composite scale that ranges from 4 to 12, where larger numbers indicate more sleep problems.
Parents’ health condition. This variable is composed of two questions. Respondents were asked if their mother or father were ever diagnosed with diabetes or high blood sugar levels. This variable is equal to 2 if both the father and mother were diagnosed with diabetes or high blood sugar, 1 if the mother or father were diagnosed, and 0 indicates that neither the father nor the mother were diagnosed with diabetes or high blood sugar.
Hypertension. This is a dichotomous variable that indicates 1 if the respondent has ever been diagnosed with hypertension or high blood pressure, 0 otherwise.
Community size. Community size is classified into four categories depending on the population size: 1) less than 2,500 inhabitants; 2) between 2,500 and 14,999 inhabitants; 3) 15,000 or more, but less than 100,000 inhabitants; 4) 100,000 or more.
Method
Hierarchical linear modeling technique is appropriate when data contains a structure of information with individuals (level 1) nested within communities (level 2). The primary focus of the analysis is on the relationship between being diagnosed with diabetes and the level-1 predictors as well as community size (level 2). Level-1 predictors are health perception, depression, exercise, sleep problems, parents’ health condition, and hypertension. Level-1 predictors were entered as group centered variables in order to obtain more accurate estimates of the intercept and to analyze the effects of the level-1 and level-2 predictor variables independently. Community size is included as a grand centered predictor. The outcome variable used here is dichotomous. Therefore, the predicted value of the outcome should lie in the interval between 0 and 1. A transformation of the level 1 predicted probability using a Bernoulli distribution is more appropriate for our data. Statistical significance was considered with p <0.05 and p <0.10. Level-1 model, level-2 model, and mixed model were estimated using Equation 1 and 2. Equation 1 and 2 present the intercepts and slopes as outcomes model using a Bernoulli distribution.
Level-1 model:
Where ηij represents the log of the odds of success
Level-2 model:
Where:
Results
Table 1 shows the descriptive statistics of the variables.
Table 1 Descriptive statistics.
| Variable | Percentage with condition | ||
| Diabetes | 25.3% | ||
| Depression | 28.1% | ||
| Hypertension | 48.1% | ||
| Exercise | 38.0% | ||
| Mean | Median | Confidence Interval | |
| Health perception | 3.30 ± 1.07 | 4 | 3.288724 -3.325261 |
| Sleep problems | 6.5981 ± 2.04 | 6 | 6.563175 -6.632942 |
| Both parents with diabetes | One parent with diabetes | None with diabetes | |
| Parents' health condition | 4.6% | 27.7% | 67.6% |
Source: own estimation with information from the Mexican Health and Aging Study, 2015. n = 13,186 cases.
Multilevel analysis allows identifying how different community sizes contribute to the explanation of variance in the probability of having diabetes. Owing to the dichotomous nature of the outcome variable, level-1 variance is heteroscedastic and the intraclass correlation (ICC) does not reveal the percentage of variance explained by community size (level-2 variable) in our model (Raudenbush and Bryk, 2002). Therefore, as a first step, we ran a logit model using the original outcome variable and community size as independent variable to ascertain the significance of the random variance component at level 2. The results suggest that the variance explained by community size across individuals is significantly greater than zero. Then, we proceeded to estimate our HLM based on a Bernoulli distribution. Table 2 shows the estimates of the intercepts, slopes as outcomes model and the odds ratio.
Table 2 Regression coefficients of having diabetes (intercepts and slopes as outcomes model)
| Fixed Effect | Coefficient | Standard error | t-ratio | p-value | Odds Ratio |
|---|---|---|---|---|---|
| Intercept,β0 | |||||
| Intercept,γ00 | -1.204143 | 0.065334 | -18.431 | .003 | 0.299949 |
| Community size,γ01 | 0.097815 | 0.056879 | 1.72 | .228 | 1.102759 |
| Health perception slope,β1 | |||||
| Intercept,γ10 | -0.138154 | 0.020791 | -6.645 | <.001 | 0.870965 |
| Community size,γ11 | 0.028546 | 0.015673 | 1.821 | .069 | 1.028958 |
| Depression slope,β2 | |||||
| Intercept,γ20 | 0.119671 | 0.053874 | 2.221 | .026 | 1.127126 |
| Community size,γ21 | 0.103538 | 0.040404 | 2.563 | 0.01 | 1.109088 |
| Exercise slope,β3 | |||||
| Intercept,γ30 | -0.290023 | 0.05012 | -5.787 | <.001 | 0.748246 |
| Community size,γ31 | 0.056279 | 0.037588 | 1.497 | .134 | 1.057893 |
| Sleep problems slope,β4 | |||||
| Intercept,γ40 | 0.055773 | 0.012245 | 4.555 | <.001 | 1.057358 |
| Community size,γ41 | -0.013192 | 0.009142 | -1.443 | .149 | 0.986895 |
| Parents’ health condition slope,β5 | |||||
| Intercept,γ50 | 0.614079 | 0.040543 | 15.146 | <.001 | 1.847954 |
| Community size,γ51 | -0.044011 | 0.030168 | -1.459 | .145 | 0.956944 |
| Hypertension slope,β6 | |||||
| Intercept,γ60 | 0.967646 | 0.049358 | 19.605 | <.001 | 2.631743 |
| Community size,γ61 | -0.040207 | 0.036999 | -1.087 | .277 | 0.96059 |
Source: own estimation with information from the Mexican Health and Aging Study, 2015.
Results indicate that as individuals have a better perception of their health condition (γ10 = -0.138154, p<.001) and do more exercise (γ30 = -0.290023, p<.001) they are less likely to have diabetes. Meanwhile, depression (γ20 =0.119671, p<.05), sleep problems (γ40 = 0.055773, p<.001), having hypertension (γ60 = 0.967646, p<.001) and parents with diabetes (γ50 = 0.614079, p<.001) are positively related to the likelihood of having diabetes.
Regarding the effect of community size, the interaction terms are significant only for perception of health condition (γ11 = 0.028546, p<.10) and depression levels (γ21 =0.103538, p<.01). Graph 1 and 2 show the effect of community size on the likelihood of having diabetes by health condition and depression level. As it can be seen, individuals living on large-sized localities are more likely to have diabetes than people residing in small communities. The difference in the slope indicates that the impact of community size is greater as individuals have a better perception of their health condition. As a consequence, the gap of probability of having diabetes is greater in smaller communities. On the other hand, the difference in probability of individuals with different perception of their health condition is lower in large-sized localities than among people residing in smaller communities. Concerning depression, the impact of depression levels on the likelihood of having diabetes increases as individuals live in large communities.
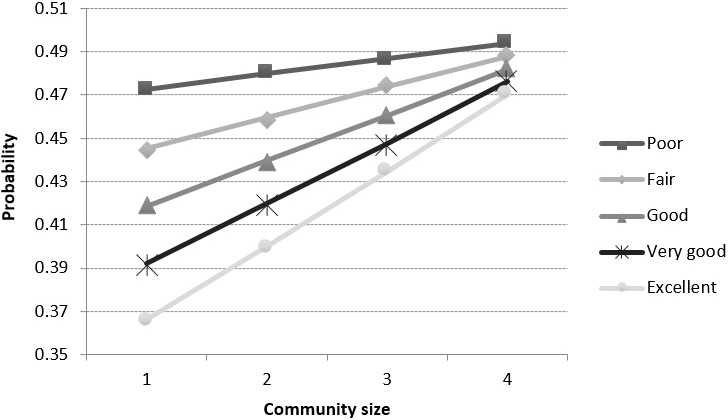
Source: own estimation with information from the Mexican Health and Aging Study, 2015.
Graph 1 Probability of having diabetes, by perception of health condition and community size.
Discussion
The question that guided the study, questioned about individual and environmental factors that favor the development of T2DM in adults 50 years and older in Mexico. The sample studied is characterized by the prevalence of T2DM coincident with that reported in ENSANUT MC (INSP, 2016, 46), with depression levels below that published in some studies with Mexican population (Martínez-Hernández et al., 2014, 105; Serrano-Becerril, Zamora-Henández, Navarro-Rojas, Villarreal-Rios, 2012, 325) an important percentage with arterial hypertension, which implies a high risk of CVD, especially for those who also suffer from T2DM (Campbell et al., 2011, 1000).
A third of those who reported having T2DM confirmed that at least one of their parents had diabetes, suggesting an imminent risk to their descendants (Cederburg, Stancakova, Kuusisto, Laakso, Smith, 2015, 550).
Even though the age range of the studied sample was wide (50 to more than 80 years), and the perception of the state of health is impoverished in the third age, perceiving a good state of health and exercising were variables that diminished the probability of having T2DM. Those who decide to exercise usually have positive psychological characteristics in terms of perception, self-esteem, self-efficacy, cognition, and emotion, which allow to assess and maintain a better state of health. Several factors can be mentioned as barriers for older adults to exercise, among them dysfunctions and functional limitations of aging (INSP, 2012, 48) environmental and social context barriers (geographical location, climate, community/neighborhood, economy). The proper factors of aging can lead to the "disability and dependence" that makes older adults susceptible to developing chronic diseases.
In the opposite direction, depression, sleep problems, arterial hypertension, and family history of first line with the disease were more likely to develop T2DM. These factors negatively influence health promoting behavior, which favors the development of diseases related to unhealthy lifestyle. It is known that depression has a bidirectional relationship with T2DM, both share environmental etiological factors and biochemical conditions. Among the first, there is socioeconomic deprivation, little social support, smoking, alcoholism, physical inactivity. Within the second, they are related to innate proinflammatory responses (cytokines), the role of the hypothalamic-pituitary-adrenal axis (HPA), the role of the circadian cycle, and insulin resistance, which interact with each other (Moulton, Pickup, Ismail, 2015, 489).
Sleep problems result in a state of daytime sleepiness that affects the performance of self-care activities (Griva et al., 2016, 7). It is also associated with an increase in proinflammatory cytokines, such as interleukin 6 and tumor necrosis factor (TNF), alteration in the nocturnal production of hormones related to satiety and the desire to eat, e.g. leptin, melatonin, ghrelin; which lead to greater predisposition of overweight, obesity and metabolic syndrome (Moulton, Pickup, Ismail, 2015, 489).
When speaking of those who do not yet have the disease, suffering from hypertension, having first-line relatives with T2DM are variables strongly associated with the development of T2DM, which is diagnosed even after the age of 60 (Zoungas et al., 2014, 2473). In addition, the tendency to worsen or present more complex health situations arise if there are over-aggregated conditions such as overweight, obesity, and arterial hypertension (Martínez-Hernández et al., 2014, 106).
Within the results of the multilevel analysis, it is identified the influence of the size of the community on the probability of having a diagnosis of T2DM. The characteristic of community size is important because it is an indicator of the type and quantity of health services available in the area, as well as the social and cultural context. According to the results of this study, the size of the community does not have a statistically significant impact on the probability of having diabetes, for variables such as family history of T2DM, arterial hypertension, sleep problems, and exercise habits. That is, people who live in small communities in Mexico and have a family history of T2DM, hypertension, sleep problems, and exercise habits, have the same probability of having T2DM than people who reside in large communities and have these same characteristics.
On the contrary, the greater the size of the community where the person resides, the greater the effect that health perception and depression will have on the probability of suffering from T2DM. In other words, individuals with a higher level of depression living in large localities will be more likely to have T2DM than those who reside in small communities. Although it could be expected that the greater accessibility to quality health services and health insurance existing in the larger communities, it is directly associated with the health status of the community beneficiary of these services or user of the same (Lee, Chen, Weiner, 2004, 1507), the results of this study indicate the contrary.
Some authors (Dunn and Hayes, 2000, 586; Gillis, 1974, 306; Matheson, Moineddin, Dunn, Creatore, Gozdyra, Glazier, 2006, 2615), point out that there are stressors that delimit the community's environment, and that in turn, have a negative effect on the health levels of the population. These stressors are aspects of the environment that condition people's lifestyles and generate demands that in turn interact with individual characteristics (Wheaton, 1999, 196). In this way, stressors may not only affect individual characteristics, but also interact continuously with these characteristics and determine the effect they will have on the possibility of suffering from T2DM. That is, aspects of urban areas, such as increased traffic, a faster pace of life, urbanization, among others, enhance the effect of the perception of health, and the presence of depression on the probability of suffering from T2DM.
When it is observed that the size of the community interacts with the perception of health and has a significant effect on the probability of having T2DM, it is clear that in the larger communities, those who perceive a poor state of health, have the highest probabilities of suffering DMT2. In this regard, the most frequent official information on health units accessible to the population, indicates a ratio of one unit per 100 thousand inhabitants. While the data used in this analysis, they defined the size of the communities with: I) less than 2,500 inhabitants; II) between 2,500 and 14,999; III) with 15,000, and more, but less than one hundred thousand; and IV) over 100,000 inhabitants. This suggests that the respondents most likely to have T2DM have low access to health services that apply preventive measures in this population group.
In this direction, the results of this study indicate that the differences in the probability of suffering from T2DM are lower among people with different health perceptions living in large communities, compared to those living in small localities. While the difference in the probability of having T2DM between a person with a poor perception of health and one with an excellent perception of health in a locality of less than 2,500 inhabitants is around 0.1, this difference in communities with more than 100,000 inhabitants is less than 0.04. These differences in the probability gaps between communities of different sizes may be due to stressors as well as the access to health services. The stressors of the larger communities interact with the individual characteristics and can generate a convergence effect in the probability of suffering T2DM among people who have a different perception of their health. In addition to the stressors that enhance the effect of health perception, access to health services can also reduce the gap between individuals who perceive their health status differently. Thus, a person with a perception of health living in conditions of poverty in a large community knows that in his/her environment there are resources for access to health services, which can improve his/her health condition, if uses them and thus have a level of health similar to the rest of the population.
The second factor that interacted with the size of the community was the presence of depression, finding that the highest probability of developing T2DM occurs in those who have higher levels of depression and living in large communities. This finding could not be attributed totally to the accessibility to health services, since it is in the large communities that they have the best hospitals and health centers (Lee, Chen, Weiner, 2004, 1508). However, the case of inaccessibility due to the right to medical care they must be insured beneficiaries, geographic location, limited economic resources, disability or functional incapacity to transport oneself autonomously and/or incompatibility of schedules (Gong, Kendig, He, 2016, 63). Also, it could be due to social factors that are important especially in this final stage of life, such as the lack of social support, the insecurity present in recent years and the social isolation that would be exacerbated by the circumstances that characterize the large urban areas. It is also possible that the elderly or third age elderly is alone most of the time because the young members of the family must leave to work, leaving him confined in his home (Brenner, Skolarus, Clarke, Burke, 2018, 70).
The findings of this research contribute to the understanding of the increase in the prevalence of T2DM in México and the design of public policies. By one side, prevention and health-disease care campaigns must move from an individual approach to a collective-based approach (Rose, 1993, 555). Although health promotion actions have intensified their emphasis on actions such as promote the exercise, eating healthy, among others; it is necessary that they consider the limitations that larger communities have and that do not allow the population to follow such recommendations of prevention. On the other side, due to the great diversity of communities in Mexico, T2DM prevention and care campaigns should incorporate regionalized actions, that is, socially adapted, because stressors can vary between communities of the same size, as well as their impact in the health of individuals. For example, a campaign that seeks to reduce the use of motorized transport to promote greater physical activity; it is likely to be more feasible to run in Mexico City than in the Metropolitan area of Monterrey due to the climatic characteristics of each region, although both areas have more than 100,000 inhabitants.
The present investigation was limited mainly by the type of existing information in database (some variables of already known importance for developing diabetes were not measured, such as age, age of diagnosis, BMI, socioeconomic level, educational level), specifically in the operationalization of the variables, depression as well as hypertension, measured as dichotomy variables that do not allow observing the effect of the variability of these on the probability of suffering from T2DM. Similarly, the health condition is measured by the perception of the respondents, which does not necessarily coincide with the definition of health used by professionals in the health area. On the other side, given the available information, in this research it was not possible to identify the impact of other contextual characteristics, beyond the size of the community (such as residence time in the communities).
One of the challenges for future research is the analysis of possible stressors (e.g. urbanization, characteristics of the community), the regionalized study of these, the impact of the variables in longitudinal terms and the inclusion of people in different stages of life. Likewise, it is important to continue exploring other characteristics of the community, beyond their size, that may affect the impact of individual characteristics on the probability of suffering from T2DM.
Conclusion
The diagnosis of T2DM can be explained from individual factors, such as depression, sleep problems, the presence of arterial hypertension, family background, poor health perception, and lack of exercise. Additionally, there are environmental conditions, such as the size of the community where people reside, which interact with specific individual factors, which enhance the development of T2DM. This allows to understand important aspects to take into account in the design and planning of health intervention, which should be socially adapted according to the proper characteristics of the community to intervene, specifically in the approach to the prevention of high-cost diseases.











 nueva página del texto (beta)
nueva página del texto (beta)



