Introduction
Tractography is used to correlate the integrity of white matter tracts with cognitive function in cognitively healthy people and with dementia1. It is a special technique of simple magnetic resonance imaging (MRI), which consists of non-invasive diffusion tensor imaging (DTI), sensitive to the diffusion of water molecules2, which allows a live three-dimensional reconstruction of the tracts within the central nervous system1,3. The fibers of white matter are classified into three categories: (a) association fibers: those that interconnect cortical areas of the same hemisphere, (b) commissural fibers: interconnect areas between both hemispheres, and (c) projection fibers, which connect the cortex with formations of lower levels4.
The interruption of the tracts can be detected as a decrease in fractional anisotropy (FA) (diffusion orientation and directionality) and an increase in mean diffusivity (MD) (degree of water diffusion)1,4,5,6. An anisotropy of 0 corresponds to a perfect sphere, while 1 would be an ideal linear diffusion. Well-defined tracts generally have an FA greater than 0.21,6,7. Preliminary studies show a decrease in white-matter connections in patients with Mild cognitive impairment and Alzheimers disease (AD). Especially noticeable is the increased MD and decreased FA in these patients compared to normal controls. These changes were found in the posterior cingulate fasciculus, the uncinate fasciculus, or both at once1.
AD is the most common neurodegenerative disorder that causes dementia in elderly individuals. The cause of AD is unknown in most cases. The most powerful risk factor for developing AD is age, with AD affecting as many as 40-50% of individuals older than 85 years8. Mixed dementia (MixD) represents the third leading cause of dementia, only behind AD and vascular dementia (VaD). The prevalence range of MixD varies between 20% and 40%9,10. The Vascular Impairment of Cognition Classification Consensus Study (VICCCS) proposes in its classification of vascular cognitive impairment (VCI) the definition of MixD, which includes phenotypes that represent the combination of vascular and neurodegenerative diseases, that is, VCI-AD, in addition to other possible combinations11. From a clinical viewpoint, loss of memory (especially episodic and semantic) is considered a typical feature of AD, whereas executive dysfunction has traditionally been associated with MixD. Several MRI analysis methods can track structural atrophy in AD and the presence of ischemic lesions on computed tomography or MRI is key in the diagnosis of individuals with MixD9.
Populations with high cardiovascular risk, patterns are more frequently observed cognitive skills of mixed type and the pure forms of dementia or sole are not the first diagnostic option in older subjects with memory complaints. This aspect is important because the adequate identification of these potentially risk factors modifiable could help intervene in an entity still without a definitive therapeutic route9. Accurate diagnosis of AD and MixD is of crucial significance for epidemiological purposes and for preventive and therapeutic strategies12.
The objective of our study was to evaluate the characteristics of white matter tracts by DTI (tractography) in elderly people with dementia type AD and MixD through the measurements of FA and MD.
Methods
Type of study and patients
Cross-sectional study carried out in a memory disorder clinic of a third-level hospital in Mexico City. All the patients were recruited in a period from March 2019 to December 2019. They all signed a consent form and underwent clinical and cognitive evaluations by a specialist in neurology and/or geriatrics. From the comprehensive geriatric evaluation, sociodemographic variables were obtained such as sex, age, education, Katz Index13, Lawton and Brody Scale14, and Yesavage Geriatric Depression Scale (GDS)15. The neuropsychological evaluation consisted of applying the NEUROPSI test16, Mini-Mental State Examination (MMSE)17, verbal fluency test18, clock-drawing test19, frontal assessment battery (FAB)20, and the Clinical Dementia Rating (CDR) Scale21.
Patients with visual and auditory acuity deficits that would make it impossible to apply neuropsychological tests were excluded, as well as patients with dysthyroidism (hyper or hypothyroidism) without treatment, hypertension, dyslipidemia and/or uncontrolled diabetes mellitus, and those with glycosylated hemoglobin levels higher than 9%, patients with severe hypoglycemia, other causes of dementia (vascular, frontotemporal, Lewy bodies), other uncontrolled medical conditions (cardiovascular, renal, or advanced lung disease), inflammatory diseases, active smokers, patients with significant depressive symptoms (GDS score > 5/15), CDR > 1, and the presence of metallic objects, devices, or conditions that would make MRI impossible.
Clinical diagnosis of dementia
The patients were classified into two groups: AD n = 8 and MixD n = 8, according to their performance in neuropsychological evaluation and current clinical criteria. For the diagnosis of dementia type AD, the criteria of the Diagnostic and Statistical Manual of Mental Disorders version 5 (American Psychiatric Association DSM-5)22 and the criteria of the National Institute of Neurological and Communicative Disorders and Stroke Alzheimers Disease and Related Disorders Association (NINCDS-ADRDA)23 were used. For the diagnosis of MixD, the VICCCS11 criteria were used. For the dementia stage, the CDR score (Mild = 1) was applied in both conditions.
Magnetic resonance DTI (tractography)
All patients had a simple brain MRI, with T1 sequence with DTI and volumetry. The images were obtained with a 1.5T resonator (Siemens® Medical Systems). Image processing was performed by the Neuroimaging Department of the National Institute of Medical Sciences and Nutrition, Salvador Zubirán (INCMNSZ). The MRI was evaluated by a neuroradiologist (not knowing of patients being in the clinical group). A high-resolution anatomical scanner was used with a T1-weighted three-dimensional magnetization sagittal sequence, prepared with fast gradient echo (MP-RAGE), field of view (FoV) 26 mm, spatial resolution 1 × 1 × 1 mm3, repetition time of 1500 ms (TR), echo time (TE), rotation angle 9°, number of cuts 176, with 25 independent diffusion gradient directions1,4,5,24. The process to perform the tractography begins with the definition of an origin point (also called seed point), and the reconstruction process, which consists of taking the orientation of the voxel and advancing a certain distance until a new direction of propagation is found with the help of the orientation of neighboring voxels. From here on, it continues iteratively, adding a new segment to each step, thus forming a path with the points in each step3,25. The basis of the anisotropic diffusion of water in the nervous system is due to the involvement of longitudinally oriented structures within the axons, such as myelin, axonal membrane, microtubules, neurofilaments, or axonal transport, which hinders the diffusion of water. MD measures the extent of diffusion in a voxel; the increase in MD may be related to a loss of coherence in fiber alignment, a lower fiber density, or a loss of myelination1,6,8.
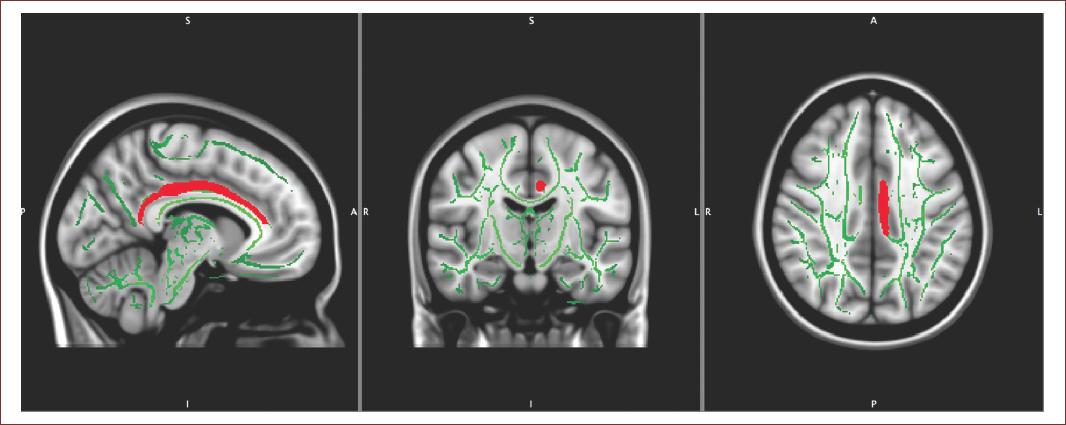
The images obtained from DTI were assigned to maps of FA and MD, the tracts were established using JHU White Matter Tractography Atlas. A standard color scheme was used in the software to encode the FA maps, with blue indicating superior-inferior, red indicating transverse, and green indicating anterior-posterior26. Tracts were created in the Diffusion Toolkit using the Continuous Tracking Fiber Assignment method with 35° angle threshold and a unique set of fibers was generated for each patient by performing anatomically detailed analysis. It was decided to study tracts that correspond to association, commissural and projection fibers (16 brains, 48 regions of interest ROI). Mean values of FA and MD were analyzed for each tract, these being the most important indices for determining dementia according to the previous studies1,6. In Figure 1, an example of the tract obtained with the proposed protocol is shown, where the cingulum is seen in red, corresponding to the left cerebral hemisphere.
Structural MRI
Cortical thickness studies
The T1 images were processed with the FreeSurfer 5.3 program, which is capable of constructing models of the cortical surface of the nervous system. This software works in an automated way and the process consists of registering the input volumes determined by the user to the atlas MNI305 (Montreal National Institute), then it performs an intensity normalization and a segmentation of the voxels according to this parameter and their spatial location to classify them in different types of tissue: gray matter, white matter, and cerebrospinal fluid27. For the present study, cerebral cortex was divided into 48 ROIs based on turns per hemisphere, and in this manner, the geometric information derived from the cortical model with the labels of the neuroanatomical parceling is incorporated.
The entire protocol was acquired during a single 25-min session, where the patients brain was aligned in the stereotactic space: the anterior commissure-posterior commissure line was aligned with the axial plane, and the interhemispheric fissure was aligned along the sagittal plane and at right angles to the coronal plane.
Statistics analysis
The variables are described by using arithmetic mean and standard deviations. The Chi-square test was used for categorical variables and the MannWhitney U test was used for continuous variables. Clinical and demographic data were tested for normality using a ShapiroWilk test. The voxel statistics in the skeletonized images were performed using the randomized, an FSL tool for nonparametric permutation inference in neuroimaging data. The carcass of mean FA (threshold 0.2) was used as a mask, the permutation number was set at 5000, meaning the difference between groups was corrected for multiple comparisons using the no-threshold cluster enhancement method (TFCE) and tested a p < 0.01. To identify the power of the selected brain areas to discriminate between AD and MixD, a stepwise discriminant analysis was performed using the dementia subgroup (AD or MixD) as the dependent variable and the mean values of ROI of FA and MD as independent variables. Finally, by means of a Spearman correlation, the differences between the characteristics of the microstructure of the brain regions were searched in FA, MD, and the neuropsychological evaluation. Variables with a value of p < 0.05 were taken as significant.
SPSS version 22 for Windows® (SPSS Inc., Chicago, Illinois) was used for the analyses. The protocol was approved by the institutional Ethics Committee (REF. 3009).
Results
The average age of the AD group members was 84.3 ± 8.8 years old and of the MixD group, it was 85.3 ± 7.6 years old (p < 0.57) and 69% were women (p < 0.23). The average schooling of AD patients was 10.2 ± 7.3 and of MixD was 11.3 ± 4.8 (p < 0.87). In the AD group, 38% were hypertensive versus 100% in MixD (p < 0.00) and none had obesity in the AD group versus 38% in MixD (p < 0.05). Regarding the global neuropsychological assessment, patients with AD had a worse cognitive performance in the cognitive assessment (NEUROPSI) 68.5 ± 11.6 points compared to the MixD group 83.2 ± 12.4 (p < 0.02) (Table 1).
Table 1 Sociodemographic characteristics and cognitive performance in Alzheimers disease and mixed dementia
| Total patients (n = 16) | Alzheimers disease (n = 8) | Mixed dementia (n = 8) | p | |
|---|---|---|---|---|
| Age years | 84.8 ± 7.9 | 84.3 ± 8.8 | 85.3 ± 7.6 | 0.57 |
| Sex (Female) % | (11) 69 | (4) 25 | (7) 44 | 0.23 |
| Years of education, % | 10.8 ± 6.0 | 10.2 ± 7.3 | 11.3 ± 4.8 | 0.87 |
| Hypertension % | (11) 69 | (3) 38 | (8) 100 | 0.00 |
| Mellitus diabetes % | (3) 19 | (1) 13 | (2) 25% | 0.52 |
| Heart disease % | (4) 25 | (1) 13 | (3) 38 | 0.24 |
| Cerebral vascular event % | (1) 6 | (0) 0 | (1) 13 | 0.30 |
| Dyslipidemia % | (9) 56 | (3) 38 | (6) 75 | 0.13 |
| Hypothyroidism % | (4) 25 | (1) 13 | (3) 38 | 0.24 |
| Obesity % | (3) 19 | (0) 0 | (3) 38 | 0.05 |
| History depression % | (4) 25 | (2) 25 | (2) 25 | 1.00 |
| GDS 15 | 2.0 ± 1.5 | 2.6 ± 1.5 | 2.2 ± 1.6 | 0.72 |
| Functionality | ||||
| KATZ | 6.0 ± 0.2 | 6 ± 0.0 | 5.8 ± 0.3 | 0.72 |
| LB | 6.5 ± 2.5 | 5.3 ± 2.9 | 5.2 ± 2.3 | 0.72 |
| NEUROPSI total | 75. 8 ± 13.9 | 68.5 ± 11.6 | 83.2 ± 12.4 | 0.02 |
| Orientation | 4.0 ± 1.7 | 5.1 ± 1.3 | 2.8 ± 1.4 | 0.02 |
| Attention | 13.8 ± 5.2 | 13.88 ± 4.9 | 13.75 ± 5.8 | 0.72 |
| Memory | 20.6 ± 5.4 | 23.3 ± 4.9 | 17.8 ± 4.7 | 0.03 |
| Language | 23.1 ± 4.1 | 21.7 ± 5.1 | 24.5 ± 2.6 | 0.23 |
| Visuospatiality/visuospatiality | 9.22 ± 1.5 | 9.1 ± 1.6 | 9.3 ± 1.6 | 0.87 |
| Executive functions | 11.5 ± 3.5 | 11.8 ± 3.6 | 11.2 ± 3.6 | 0.50 |
| MMSE | 22.5 ± 3.2 | 22.6 ± 3.2 | 22.5 ± 3.5 | 0.03 |
| Semantic verbal fluency (animals) | 11.0 ± 3.8 | 13.0 ± 2.8 | 9.1 ± 3.8 | 0.06 |
| Phonological verbal fluency (letter F) | 8.9 ± 3.8 | 10.6 ± 4.0 | 7.0 ± 3.5 | 0.05 |
| Clock-drawing test | 2.3 ± 1.7 | 2.5 ± 2.0 | 2.13 ± 1.3 | 0.95 |
| FAB | 12.4 ± 3.2 | 12.88 ± 3.9 | 12.0 ± 2.5 | 0.44 |
GDS - 15: Yesavage Geriatric Depression Scale; LB: Lawton and Brody scale; MMSE: Mini-Mental State Examination; FAB: front evaluation battery.
DTI (Tractography)
Regarding the tractography findings, significant differences were found in FA between the AD versus MixD groups in the following tracts: right cerebral peduncle 0.5733 versus 0.5557 (p < 0.05), left cerebral peduncle 0.5744 versus 0.5476 (p < 0.01), right external capsule 0.3619 versus 0.3346 (p < 0.01), and left cingulum gyrus 0.4049 versus 0.3756 (p < 0.05). Regarding MD, the differences found were in the following tracts: right thalamic posterior radiation 0.0016 versus 0.0010 (p < 0.03) and capsule left external capsule 0.0015 versus 0.0012 (p < 0.03) (Table 2).
Table 2 Comparison of tracts, fractional anisotropy, and mean diffusivity in Alzheimers disease and mixed dementia
| Total Patients (n = 16) | Alzheimers disease (n = 8) | Mixed Dementia (n = 8) | p | |
|---|---|---|---|---|
| Fractional anisotropy | ||||
| Right cerebral peduncle | 0.5645 ± 0.0172 | 0.5733 ± 0.0176 | 0.5557 ± 0.0121 | 0.05 |
| Left cerebral peduncle | 0.5610 ± 0.0215 | 0.5744 ± 0.0209 | 0.5476 ± 0.0121 | 0.01 |
| Right external capsule | 0.3483 ± 0.0246 | 0.3619 ± 0.0246 | 0.3346 ± 0.0163 | 0.01 |
| Left cingulum gyrus | 0.3902 ± 0.0271 | 0.4049 ± 0.0224 | 0.3756 ± 0.0241 | 0.05 |
| Mean diffusivity | ||||
| Right thalamic posterior radiation | 0.0013 ± 0.0004 | 0.0016 ± 0.0005 | 0.0010 ± 0.0000 | 0.03 |
| Left external capsule | 0.0013 ± 0.0003 | 0.0015 ± 0.0003 | 0.0012 ± 0.0001 | 0.03 |
Correlations between cognitive domains and DTI parameters
A correlation was observed between the cognitive domains and the tractography parameters (FA and MD) in both groups, finding a moderate correlation in the AD group between orientation and left cerebral peduncle with a Rho of 0.72 (p < 0.04); in the MixD group between orientation and left cingulate gyrus with a Rho of 0.73 (p < 0.04), memory and left cerebral peduncle with a Rho of −0.70 (p < 0.05), and phonological fluency and left cerebral peduncle with a Rho of −0.72 (p < 0.04) (Table 3).
Table 3 Spearman correlation between neuropsychological testing and DTI parameters in Alzheimers disease and mixed dementia
| Alzheimers disease | Mixed dementia | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Orientation | Memory | Fluency phonological | Orientation | Memory | Fluency phonological | |||||||
| Rho | p | Rho | p | Rho | p | Rho | p | Rho | P | Rho | p | |
| Fractional anisotropy | ||||||||||||
| Right cerebral peduncle | 0.31 | 0.44 | 0.03 | 0.93 | −0.10 | 0.81 | 0.11 | 0.78 | −0.32 | 0.43 | −0.36 | 0.37 |
| Left cerebral peduncle | 0.72 | 0.04 | 0.07 | 0.86 | −0.07 | 0.86 | −0.27 | 0.51 | −0.70 | 0.05 | −0.72 | 0.04 |
| Right external capsule | 0.34 | 0.40 | −0.27 | 0.50 | −0.35 | 0.39 | 0.07 | 0.85 | −0.18 | 0.67 | −0.44 | 0.26 |
| Left cingulum gyrus | 0.60 | 0.11 | −0.10 | 0.79 | −0.12 | 0.76 | 0.73 | 0.04 | 0.25 | 0.54 | 0.32 | 0.43 |
| Mean diffusivity | ||||||||||||
| Right thalamic posterior radiation | −0.16 | 0.69 | −0.12 | 0.77 | −0.10 | 0.81 | −0.39 | 0.33 | 0.24 | 0.56 | 0.21 | 0.60 |
| Left external capsule | −0.46 | 0.25 | −0.20 | 0.62 | −0.12 | 0.76 | −0.54 | 0.16 | −0.46 | 0.24 | −0.27 | 0.50 |
Cortical thickness studies
In the volumetric analysis, significant differences were found in the following ROIs between AD and MixD: Brain segmentation volume 964.92 cm3 versus 877.95 cm3 (p < 0.02), brain segmentation volume without ventricles 904.25 versus 837.76 (p < 0.01), brain segmentation volume without ventricles from surf 903.46 versus 837.16 (p < 0.01), right hemisphere cerebral white matter volume 184.52 versus 168.32 (p < 0.03), subcortical gray matter volume 46.06 versus 42.10 (p < 0.05), total volume of gray matter 514.03 versus 479.94 (p < 0.01), total intracranial volume 1471.92 versus 1324.38 (p < 0.05), left thalamus 5.86 versus 5.37 (p < 0.02), left caudate 3.5 versus 2.71 (p < 0.02), fourth ventricle 2.14 versus 1.54 (p < 0.05), right caudate 4.01 versus 2.90 (p < 0.02), and right choroid plexus 0.92 versus 0.71 (p < 0.03) (Table 4).
Table 4 Volumetry in regions of interest in Alzheimers disease and mixed dementia
| Total patients (n = 16) | Alzheimers disease (n = 8) | Mixed dementia (n = 8) | p | |
|---|---|---|---|---|
| Brain segmentation Volume, cm3 | 921,44 ± 76.83 | 964.92 ± 69.93 | 877.95 ± 58.61 | 0.02 |
| Brain segmentation volume without ventricles, cm3 | 871.00 ± 58.93 | 904.25 ± 47.37 | 837.76 ± 51.68 | 0.01 |
| Brain segmentation volume without ventricles from surf, cm3 | 870.31 ± 58.87 | 903.46 ± 47.38 | 837.16 ± 51.67 | 0.01 |
| Right hemisphere cerebral white matter volume, cm3 | 176.42 ± 16.08 | 184.52 ± 14.60 | 168.32 ± 13.83 | 0.03 |
| Subcortical gray matter volume, cm3 | 44.08 ± 3.81 | 46.06 ± 3.36 | 42.10 ± 3.30 | 0.05 |
| Total volume of gray matter, cm3 | 496.99 ± 34.42 | 514.03 ± (24.91) | 479.94 ± 35.42 | 0.01 |
| Total intracranial volume, cm3 | 1398.15 ± 150.91 | 1471.92 ± 118.28 | 1324.38 ± 149.58 | 0.05 |
| Left thalamus, cm3 | 5.62 ± 0.43 | 5.86 ± 0.39 | 5.37 ± 0.33 | 0.02 |
| Left caudate, cm3 | 3.11 ± 0.69 | 3.5 ± 0.64 | 2.71 ± 0.47 | 0.02 |
| Fourth ventricle, cm3 | 1.84 ± 0.53 | 2.14 ± 0.45 | 1.54 ± 0.45 | 0.05 |
| Right caudate, cm3 | 3.45 ± 0.10 | 4.01 ± 0,24 | 2.90 ± 0.51 | 0.02 |
| Right choroid plexus, cm3 | 0.82 ± 0.25 | 0.92 ± 0.27 | 0.71 ± 0.21 | 0.03 |
Discussion
Our study compared patients with AD and MixD through a standardized acquisition protocol to investigate the parameters of FA and MD in terms of changes in the anisotropy or magnitude of water diffusion throughout the brain, demonstrating that patients with AD have alterations in specific tracts, such as right and left cerebral peduncle, right and left external capsule, left cingulate gyrus, and right thalamic posterior radiation compared to patients with MixD.
Palesi et al. demonstrated in a tractography study in patients with DVa, AD, and a control group that patients with AD had a greater affection in the parahippocampal tracts and in the knee of the corpus callosum, while patients with DVa showed a greater affection of white matter in thalamic radiation28. Reginold et al., in a study which objective was to evaluate the affection of white matter in patients with AD, demonstrated a greater commitment in the superficial white matter of the temporal lobe than in the members of a control group25.
Tu et al. compared DTI parameters in members of a control group, patients with AD and subcortical ischemic vascular disease (SIVD; also called lacunar infarction), reporting a global decrease in FA in patients with SIVD; while in patients with AD, the alterations were in the left superior longitudinal bundle, knee and splenium of the corpus callosum, anterior thalamic radiation, uncinate bundle, and left cingulate gyrus, suggesting that DTI is effective in distinguishing patients with early stage of AD versus SIVD29. Another study by Lee et al., which compared control group members, patients with MCI and AD, showed that the latter group had a greater decrease in FA, as well as lower integrity of white matter associated with a lower hippocampal volume, indicating that the pathology in white matter follows the same degree of stages and progression of neurodegeneration30.
Another finding in our study was the combined affection of tracts corresponding to neurodegeneration (turn of the left cingulum, cerebral peduncles)31, as well as areas related to the vascular component (thalamic radiation)25, a combination only observed, in our study, in patients with MixD. These alterations are the result of changes in axonal density and myelination since the homogeneity in the orientation of the axons affects the degree of FA and MD in DTI, so a decrease in FA and an increase in MD reflect a decrease in the integrity of the brain tissue1,6,32. An important aspect to consider is the fact that the vascular load in white matter in patients with MixD could be a potential confounder, similar to other DTI studies in neurodegenerative diseases.
In relation to the results of volumetry, a lower volume was observed in twelve ROIs in patients with MixD. Some studies have established a correlation between DTI parameters and volumetric parameters, indicating that these are measures of the same pathological process, that is, neurodegeneration33. The relative change in the parameters that reflect cortical integrity and diffusion is likely to vary not only depending on the methods used but also on the particular morphological process, the anatomical region being studied, and possibly the underlying molecular pathology of the disease in particular27. One aspect of techniques for detecting changes in white matter tracts is that they are more sensitive than measurements of cortical thickness or integrity; this is justified because the loss of cortical volume in neurodegenerative disease probably represents the loss of individual neurons (soma) and neuropil (corresponding dendrites, axons)4,28.
Regarding the cognitive domains and the affected tracts, we found an association between FA and orientation (left cerebral peduncle) in patients with a diagnosis of AD; this anatomical structure is considered a vulnerable area from the vascular point of view34, in addition, it is related to changes in AD29. An association was also observed between FA and the orientation domains (left cingulate), as well as in-memory and phonological fluency (left cerebral peduncle) in patients with MixD; these findings show that there is a disconnection of areas related to cortical memory (left cingulate) since this structure is a fundamental part of the limbic system and one of the main fascicles of white matter that connects areas of cortical association35.
Our results suggest that DTI allows the identification of alterations in specific tracts (cerebral peduncle and cingulate) in patients with AD compared to patients with MixD. This shows that MixD shares a spectrum of neurodegeneration (due to the affection of classic tracts affected in AD) but with alterations (decrease) in FA.
The limitations of our study are based on the cross-sectional design, which does not allow the interpretation of the causal mechanisms underlying the associations of MRI and cognitive measurements. Another important aspect is the size of the sample since this could limit the ability to detect more differences in DTI between patients with AD and MixD. Although there are various computer programs available that allow tractography to be carried out, some even free to use for research purposes, the results obtained with one or the other may vary, either due to the algorithm they use or due to their processing, since the reproducibility depends to some degree on the users interaction with the computer program. In multicenter studies, there are also variations due to different MRI equipment and the protocol used to acquire DTI images; these can influence the quantification of the results using tractography, as mentioned by Fischer et al. and Heiervang et al., who found differences in the quantification of the cerebral fascicles applying different diffusion gradients.
Our study has several strengths: it is the first study to describe tractography characteristics and their association with cognitive performance in elderly adults with AD and MixD. Our findings could lead to future studies in which MixD can be characterized better and the role of tractography and volumetry can be understood more clearly.
Our results support existing findings reported in the literature and, most importantly, provide a complete interpretation of microstructural alterations in the white matter through the spectrum of dementia type AD and MixD using the tractography technique with parametric analysis, and it could provide a useful standard for the early diagnosis of AD and MixD in the future.











 nueva página del texto (beta)
nueva página del texto (beta)