Introduction
Interatrial blocks (IABs) include a variety of disturbances in interatrial conduction and are the most frequent and well-known blocks at the atrial level1. IAB is more frequently found in elderly patients (with a prevalence of 8% in septuagenarians) and patients with structural heart disease2. These rhythm abnormalities result in varying refractory periods and slower conduction velocities within the atrial myocardium, a potential substrate for the development of atrial arrhythmias.
IABs are classified as (Fig. 1)1:

Figure 1 Classification of typical atrial block. A: partial interatrial block (first degree): P wave duration >120 ms but there is no typical biphasic morphology in II, III, and aVF (red star). B: intermittent interatrial block (second degree): Note how the P wave switches from type II atypical IAB by morphological criteria (black stars), given by biphasic P waves in III and aVF, to a normal intermittent atrial conduction with the disappearance of the negative component in II, III, and aVF (red star). C: advanced atrial block (third degree): P wave >120 ms with a biphasic component in II, III, and aVF (red star).
– Partial IAB (first degree): The ECG shows that the P-wave duration is ≥ 120 ms, and usually is bimodal (“notched”) in leads I, II, III, and aVF.
– Advanced IAB (third degree): The diagnosis is made when a P-wave duration is ≥ 120 ms, and the morphology of the P-wave in the inferior leads (II, III, and aVF) is biphasic or “positive-negative.”
– Intermittent IAB (second degree): IAB may occur transiently on a beat-to-beat basis or associated with changes in heart rate or following pauses induced by premature contractions. The P-wave morphology may show transient morphology changes in the same recording.
Advanced IAB is an increasingly recognized surrogate of atrial dysfunction and a trigger of atrial dysrhythmias, mainly atrial fibrillation (AF)3. The combination between IAB and supraventricular arrhythmias is known as Bayes’ syndrome1.
Recent studies have demonstrated a strong relationship between IAB or Bayes’ syndrome and thromboembolic phenomena, with cardiovascular and neurological consequences. Regarding neurological involvement, patients with IAB or Bayes’ syndrome have an increased incidence of ischemic events, cognitive impairment, and dementia4-6. These observations triggered the hypothesis that the early use of anticoagulation and antiarrhythmic therapy could have benefits in patients with IAB before the documentation of AF7.
This review aims to summarize the most recent evidence describing the association of IAB (and Bayes’ syndrome) with neurological events, focusing on stroke, dementia, and cognitive impairment. Potential early therapeutic options to prevent these undesirable clinical consequences will also be discussed.
IABs and stroke
Cardiac embolism is a common cause of ischemic stroke. Pathophysiological mechanisms that can explain the link between IABs and stroke are multiple and are mainly related to the potential development of supraventricular arrhythmias and impaired left atrium contractility7.
Advanced IAB was shown to be a significant predictor of both new-onset and recurrent AF3. As is known, AF is one of the most frequent causes of stroke and can be detected in nearly 25% of all patients with stroke by sequentially combining different electrocardiographic methods8. The rationale for the association between IAB and AF is probably related with atrial remodeling and fibrosis seen in both conditions; in IAB the delayed left atrium activation produces an abnormal contraction against a closed mitral valve, increasing left atrium pressure. This leads to progressive dilation, more fibrosis, an increase in pro-inflammatory markers and favors the occurrence of AF4.
Furthermore, IAB has shown to be a predictor of embolic stroke even when there is no documentation of AF9. In a big-scale study, the incidence of ischemic stroke was more than two-fold in patients with advanced IAB as compared to those without, even after the adjustment for traditional risk factors and symptomatic AF10. Similar investigations found a significantly high frequency (between 61 and 80%) of IAB in patients with sinus rhythm and a history of stroke11,12. This link between stroke and IAB in the absence of documented AF (or other atrial arrhythmias) can be explained by the specific electromechanical disorders in this condition. In advanced IAB, depolarization follows a caudo-cranial route, first toward the AV node and then in a retrograde direction through the left atrium resulting in poor left atrial electromechanical function13. This impaired functioning of the left atrium can predispose to clot formation and embolic phenomena, even in the absence of other atrial arrhythmias.
The association between advanced IAB and stroke has been demonstrated in different settings and conditions, including the general population, very elderly patients, and patients with high CHADS2 score4,14. Also in patients with a history of an embolic stroke of unknown source, advanced IAB predicted the recurrence of a cerebrovascular event15.
The detection of IAB should be considered in the risk stratification of patients in sinus rhythm that are at high risk of stroke, even if they have no documented AF. In addition, in patients that present with ischemic stroke and IAB is present in the ECG, the search for AF must be intensified9.
IABs and silent cerebrovascular disease
Clinical implications of silent cerebrovascular disease include an increased risk for future symptomatic ischemic stroke, memory impairment, and cognitive decline. At least two publications reported the association between IAB and silent brain infarctions.
In a case–control study, IAB was significantly associated with the incidence of asymptomatic cerebrovascular disease using Magnetic Resonance Imaging (MRI) examination. IAB was present in 59% of the patients with silent brain ischemia. Older age, uncontrolled hypertension, and higher CHA2DS2-VASc were significantly more common in patients with silent vascular disease16.
A cross-sectional study observed an association between advanced IAB and the total burden of asymptomatic cerebral small vessel disease in 499 patients with no documented AF. This association was independent of left atrium diameters, left ventricle ejection fraction, left ventricle wall thickness, and other possible confounding factors. Interestingly, this study constructed a small vessels disease score to better represent the burden of cerebral damage, instead of a single MRI manifestation17.
Screening for IAB might help to improve risk stratification of individuals at an elevated risk of subclinical cerebrovascular diseases.
IABs and cognitive impairment
The association of AF with cognitive impairment and dementia has been previously described18. In patients in sinus rhythm with IAB and in those with Bayes’ syndrome the association seems to be very similar. In fact, recently published data confirm the association of P-wave duration with cognitive impairment and dementia19. Pathophysiological mechanisms that explain these associations are probably multifactorial and include symptomatic ischemic stroke and silent cerebral infarcts, but also hemorrhages and hypoperfusion due to hemodynamic alterations that lead to reduced cardiac output and decreased diastolic cerebral arterial flow4,20.
In the prospective BAYES registry, which included patients aged 70 years and older with structural heart disease in sinus rhythm, an association (independent of age, sex, and other confounding factors) between IAB and cognitive impairment was found5. Interestingly, the relationship between IAB and cognitive impairment was also present during follow-up and was independent of AF and the history of stroke.
The Advanced Characterization of Cognitive Impairment in Elderly with IABs (CAMBIAD study) was a case–control multicenter study conducted in 265 subjects aged 70 years and older in sinus rhythm without significant structural heart disease. This study included 143 cases with mild cognitive impairment (Mini-Mental State Examination score 20-25) and 122 controls with normal cognitive function. Patients with cognitive impairment had longer P-wave duration, higher prevalence of IAB, and higher prevalence of advanced IAB when compared to controls. IAB was independently associated with mild cognitive impairment, both for partial and advanced IAB but with a stronger association in the case of advanced IAB21.
An association with dementia has also been suggested, particularly in patients with advanced IAB2. In the Cardiac and Clinical Characterization of Centenarians study, the prevalence of dementia progressively increased when passing from normal P-wave, to partial IAB, advanced IAB, and AF. Therefore, a systematic assessment of the cognitive status at baseline and during follow-up in patients with advanced IAB or Bayes’ syndrome should be considered2.
Role of early therapeutic interventions
The rationale of considering anticoagulation in patients with IAB and no documentation of AF relies on several observations. First, some studies using implantable devices have demonstrated a lack of a clear temporal relationship between cryptogenic stroke and paroxysmal AF, supporting the hypothesis of the importance of a prothrombogenic state in the left atrium, even in the absence of AF22. Furthermore, advanced IAB and AF share multiple clinical and pathophysiological similarities; both processes present the same anatomical substrate (fibrotic atrial cardiomyopathy) (Fig. 2), which can induce blood stasis, hypercoagulation, and more atrial fibrosis7,23,24. Finally, IABs have demonstrated to be a risk factor for stroke and cerebrovascular diseases even in the absence of AF9-12.
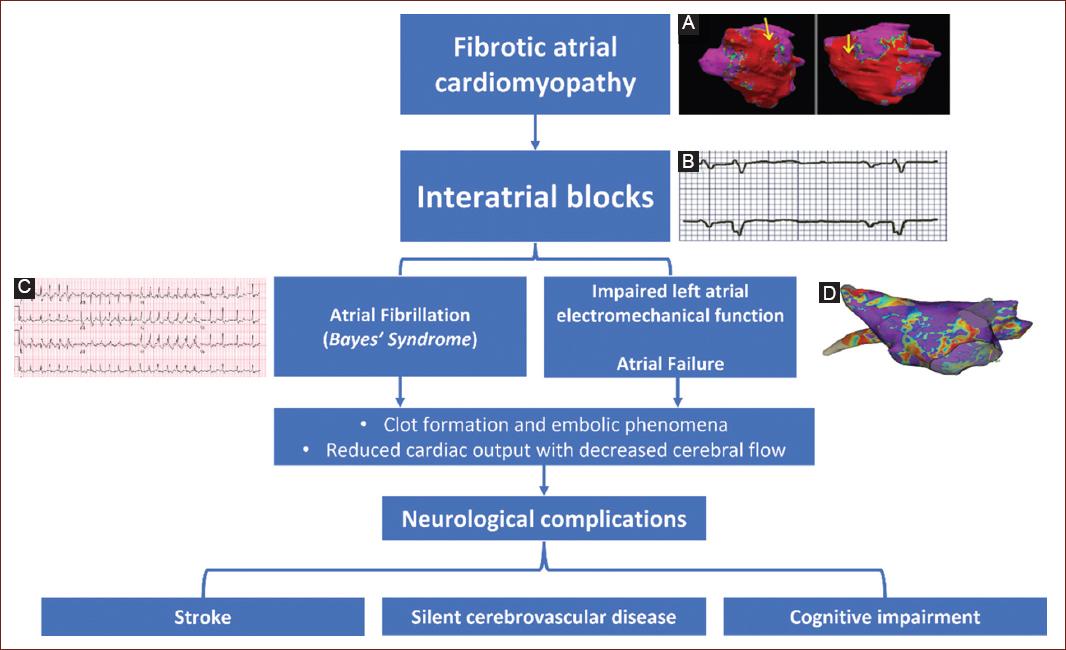
Figure 2 Neurological manifestations of interatrial blocks. Schematic diagram on the causes and mechanisms of neurological manifestations in interatrial blocks. A: three-dimensional reconstruction of a cardiovascular magnetic resonance showing extensive biatrial fibrosis. The image depicts the degree of fibrosis in a color scale (dense fibrosis in red). B: advanced interatrial block. Note the characteristics of the P wave, with a duration >120 ms and a biphasic component. C: atrial fibrillation as one of the finals manifestations of electrical and anatomical abnormalities in the left atrium. D: evidence of atrial fibrosis in a bipolar three-dimensional mapping of the left atrium. Purple color represents normal tissue colored areas (yellow, green, blue, and red) correspond to low-voltage fibrotic tissue.
There are ongoing studies aiming to compare the efficacy of anticoagulation in patients with advanced IAB with no prior documentation of AF. The results of these studies will allow determining the efficacy of this early therapeutic intervention in patients with advanced IAB and no demonstrated AF. If positive results are found, a global strategy for anticoagulation to prevent stroke in patients without AF should be considered.
Regarding antiarrhythmic treatment in IAB with no AF documentation the current situation is similar. Considering the clear and strong association of IAB with atrial arrhythmias, the idea of considering antiarrhythmic treatment when IABs are detected seems reasonable. Indeed, this idea was suggested in a small series, and anti-arrhythmic treatment of patients with advanced IAB has shown to reduce AF occurrence13,25. However, no randomized data are available at present times and whether antiarrhythmic treatment should be used to prevent arrhythmias in asymptomatic patients with IAB needs still to be tested in large prospective trials.
Conclusion
The presence of IABs is strongly associated with negative neurological consequences, mainly as a result of cardioembolic events. These conduction abnormalities need to be included in the diagnosis work-up when there is no clear cause for neurological symptoms. The use of early anticoagulation and antiarrhythmic treatment to prevent these undesirable consequences needs to be further evaluated in large trials.











 text new page (beta)
text new page (beta)


