Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Archivos de neurociencias (México, D.F.)
versão On-line ISSN 1028-5938versão impressa ISSN 0187-4705
Arch. Neurocien. (Mex., D.F.) vol.9 no.2 Ciudad de México Jun. 2004
Arch Neurocien 2004; Vol. 9(2):114-119
TEMA SELECTO
Dementia pugilistica 1a. parte
ENRIQUE OTERO SILICEO
JOEL PADILLA RUBIO
Neurology Subdirection, Manuel Velasco Suárez National Neurology and Neurosurgery Institute,
Mexico.
Correspondence shoul be send to:
Enrique Otero Siliceo
Manuel Velasco Suárez, National Neurology and Neurosurgery Institute.
Insurgentes Sur No. 3877. Col. La Fama.
14269 México, D.F.
Recibido: 1 septiembre 2003
Aceptado: 26 septiembre 2003
RESUMEN
Aunque los deportes se consideran como impulsores de salud física y mental, en el boxeo amateur o el profesional en que no se usa protección se pueden presentar lesiones agudas y crónicas del cerebro debidas al trauma y las pequeñas y grandes hemorragias que se pueden causar al cerebro. Entre ellas el Parkinson y las alteraciones psiquiátricas.
PALABRAS CLAVE: boxeo, lesiones, alteraciones.
ABSTRACT
Sports is considered a synonym for body and mind health. However, the so called contaet sports, the main example being boxing, more or less go beyond this definition.
Contemporary boxing is a spetacle, who is a continuation of historical fights of gladiators. For many years, several complications and head alterations have been related to boxing involving both the face and the skull. And, because of their outcome, some of the most important alterations are neuropsychiatric such as dementia pugilistica. A review of the available records indicates that there have been a substantial number of fatalities in primarily professional but also amateur boxers due to intracranial injuries sustained in the ring in comparison to the numbers of boxers at risk.
Dementia pugilistica is the result of chronic traumatic brain injury referred to as the neurological disorder due to repeated head injuries. About 20% of professional boxers show manifestations of chronic traumatic brain injury compared to amateur boxers where this incidence is lower because of less physical exposure due to head protection and the reduced number of rounds in fights as well as the stringent safety rules on the ring. Several risk factors to develop chronic traumatic brain injury are known. There is also a body of knowledge on the possible pathophysiological bases and pathological characteristics of chronic traumatic brain injury from brain biopsies where a similarity to Alzheimer's disease is found. The clinical picture involves neuropsycchiatric disorders such as cognitive, behavioral, and thinking alterations as well as Parkinson's like motor alterations. Diagnosis is based on the history of exposure as a boxer, neuropsychiatric studies, an EEG, a CAT sean and MRI.
KEY WORD: boxing, lesion, brain injury, Parkinson.
Sports are considered a synonym for body and mind health. However, the so called contact sports, the main example being boxing, more or less go beyond this definition. For many years, several complications and head alterations have been related to boxing involving both the face and the skull. And, because of their outcome, some of the most important alterations are neuropsychiatric such as dementia pugilistica.
Dementia Pugilistica (DP), also known as the Punch Drunk Syndrome or chronic traumatic encephalopathy, is a chronic traumatic brain injury (CTBI) combined with cumulative neurological consequences of repeated head injuries 1,2. In 1984, the British. Medical Association showed clinical, radiological and neuropsychological evidence of brain damage in boxers. Sometimes the damage was very severe and became permanent 3.
Chronic traumatic brain injury has been described more among professional active and retired boxers, and, less in other athletes playing other contact sports such as football, soccer, hockey on ice, and many martial arts disciplines.
EPIDEMIOLOGY
For more than 70 years, chronic brain damage has been described in boxers exposed for a long time to this sport. Findings determined that 20% of professional boxers have chronic traumatic brain injury without specifying whether they were professional or amateurs, or if their exposure to trauma was diminished by the use of head protection, smaller number of fight rounds 1 and stringeht ruIes on ring safety demanded for amateur boxers 16. In a medical and statistical report on professional boxers in New York State, 3110. rounds were registered between 1982 and 1984. Of these, 376 brain injuries were reported with 262 having structural brain damage. Accordingly, 0.8 brain injuries occurred per 10 rounds; 2.9 brain injuries per 10 boxers, and 1 death due to acute brain damage 17. Mortality is uncommon in the ring both among professional and amateur boxers. World literature reports 335 deaths in boxing between 1945 and 1979, i.e. 9 to 10 deaths per year 18. Death, however, was less frequent among amateur boxers with only one third of deaths among them. Some of the risk factors for chronic traumatic brain injury are: boxer retirement after 28 years, boxing for over 10 years, and participating in 150 or more fights 1. Other risk factors are exposure to sparring, a history of knock outs 4, poor physical training 5, and the associated apolipoprotein E (APO E) genotype 6-9.
PATHOPHYSIOLOGY
In spite of new findings in neuroimaging, biochemistry and molecular biology, the specific pathophysiological mechanism for chronic traumatic brain injury is unknown. However, several possible mechanisms have been proposed.
1. Martland described a mechanism in 1928 whereby repeated hitting or head injuries resulted in petechial bleeding in the deep portions of the brain inducing gliosis or a progressively degenerating injury. Thus, these signs and/or symptoms should be expected to appear in early boxing practice 13. However, even among boxers retiring from their pugilistic career and experiencing neuronal losses, the characteristic clinical data of this syndrome are not evident. This theory would explain why chronic traumatic brain injury selms to progress after head injuries cease and only when the boxer retires.
2. A second theory is about local changes in the blood brain barrier resulting from head injury leading to serum protein extravasation while triggering a secondary immune response 11 or the deposition of amyloid beta protein in sites with brain damage 12.
3. Boxer brain damage results from accelerating and decelerating the brain inside the skull, particularly rotational acceleration. This results in parenchymal and blood vessel stretching and in linear acceleration producing focal lesions 15. The strength from a hit is directIy proportional to the glove mass and to the velocity of the hit, while being inversely proportional to the total mass opposing the hit 19.
There is evidence suggesting that the presence of apolipoprotein E APOE ε4 allele promotes amyloid deposition in individuals experiencing brain damage 38. Mayeaux et al. found a synergistic risk ten times higher than Alzheimer’s disease in individuals with chronic traumatic brain injury combined with APOE ε4 that is present. In studying 30 active and retired boxers, it was found that APOE ε4 is associated to an increased severity of chronic traumatic brain injury among highly exposed boxers (boxers with over 12 professional fights). Such findings suggest this could be a genetic predisposition for an unfavorable neurological effect of a long boxing career 40. Seliger et at 41. noticed that patients with the APOE ε4 allele experienced a poorer outcome than those without the allele, especially in cognitive functions but not in motor functions.
PATHOLOGY
Neuropathological observations reported by Corsellis et al 20, 21 described four kinds of changes in the Central Nervous System in 15 former boxers, namely septal and hypothalamic anomalies, cerebellar changes, degeneration of the substantia nigra, and the regional presence of Alzheimer's neurofibrillary tangles. In twelve cases, a fenestrated cavum septi was reported. Often, the hypothalamic floor seems to be enlarged, the fomix and mammilary corpora atrophied, and the cerebellum having a reduced number of Purkinje's cells on the lower surface. Alzheimer's neurofibrillary tangles are found in the gray matter of the hippocampus and the mid-temporal region. The substantia nigra shows loss of pigment and gliosis. Histological abnormalities in chronic traumatic brain injury are similar to those found in Alzheimer's disease, but in a study by Hof et al 22, where the brains of 3 patients with dementia pugilistica and 8 patients with Alzheimer's disease were analyzed post-mortem, a difference was found in the laminar distribution ofthe Alzheimer's neurofibrillary tangle neocortex. Hence, in dementia pugilistica Alzheimer's neurofibrillary tangles prevail on the surface layers (II and III) while in Alzheimer's disease, they are located both on the surface and the deeper layers, with a greater density seen in deep layers. Alzheimer's neurofibrillary tangles are stained for the microtubule antibody associated to protein 1. The presence of positive t structures means that an abnormal deposition of this protein also occurs in dementia pugilistica. Thus, traumatic head injury has been shown to be epidemiologically a risk factor in Alzheimer's disease 25,26. Another significant neuropathological observation is the presence of ubiquitin in Alzheimer's neurofibrillary tangles in brains of boxers with dementia and in brains with Alzheimer's disease 27. Uhl et al. show evidence of similarities between chronic traumatic brain injury and Alzheimer's disease resulting in reduced cholinergic activity in a boxer with dementia pugilistica 28.
CLINICAL PICTURE
Recent studies showed evidence of neuron dysfunction in boxers. According to a detailed review by Roberts 14, multiple systems are seen altered in clinical findings of chronic traumatic brain injury involving the cerebellum, pyramidal and extrapyramidal symptoms, cognitive alterations, and behavioral changes. These become obvious after a fighter retires from boxing, albeit the precise period of time needed for chronic traumatic brain injury to develop after its onset, varies from the moment the boxer retires. Examinations on retired boxers after 50 years of age are more likely to show altered neurological findings 13.
The onset of clinical manifestations of chronic traumatic brain injury is always gradual. They usually occur as altered affective expressions and some psychotic symptoms. Early motor alterations include dysarthria and mild balance problems. Motor abnormalities progress with ataxia, spasticity, altered coordination, and Parkinson's. Developed amnesia associated to parkinsonism signs is not uncommon. Finally, patients may develop general cognitive alterations especially in terms of attention, memory, frontal and executive functions. Earlier chronic traumatic brain injury manifestations may include diminished attention followed by slow thinking and mild deficits in memory, attention and executive skills. As deterioration progresses, dementia becomes more evident expressed as amnesia, deep attention deficit, markedly slow thinking, altered judgment, rationing and planning 1. The most common behavioral disorders found are lack of inhibition, irritability, euphoria and/or hypomania, perspicacity, paranoia, explosiveness, and violence. The clinical course may stop in any of these stages while the severity of the syndrome could correlate with or be proportional to the time the boxing career lasted and the total number of fights 5,14.
DIAGNOSIS
The best method to detect cognitive abnormalities and potential brain damage is by neuropsychometry. The study must be conducted among all boxers, since they are amateurs, to diagnose the first neuropsychiatric alterations according to Finnish 16.
Neuropsychological testing is useful as an important adjuvant tracking method to assess chronic traumatic brain injury in retired boxers and in active amateur and professional boxers. Often, neuropsychological testing in amateur boxers shows fewer alterations than in professionals 29 . The picture showing that the onset of chronic traumatic brain injury can be attributed to boxing may be classified as probable, possible or improbable 30. (See table 1)
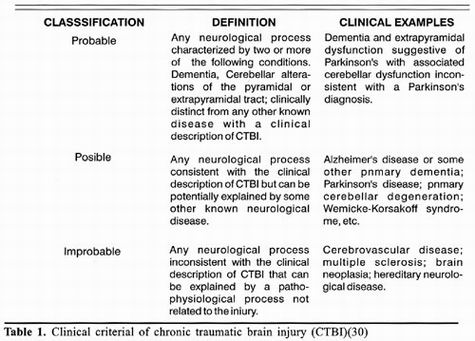
The scale to assess chronic brain damage in boxing (6) evaluates three neurological issues such as motor, cognitive and behavioral aspects with a score on a ten point scale. (See Table 2); When the neurological examination is normal, the score is zero, and mild chronic traumatic brain injury gets 1 to 2 points. Clinically, it is related to instability, mild lack of coordination, dysarthria, and memory and attention deficits. The moderate grade has a 3 or 4 point score, while the severe grade has a score higher than 4 points.

Traditionally, electroencephalography (EEG) has been the neurodiagnostic test of choice to assess brain damage in boxers. EEG, however, could be normal or show non specific findings such as trace slowing down. The frequency of abnormal EEG's among boxers with chronic traumatic brain injury is similar to that of those with no clinical evidence of chronic traumatic brain injury. In a study conducted by Greg McLatchie et al., 40% of boxers showed abnormalities mainly of the slowness type and this abnormality were not proportionately correlated to the number of fights 31. EEG is a non specific test to draw a conclusion on boxing encephalopathy but it can show progressive alterations when taken serially.
Several studies have shown the superiority of Magnetic Resonance Imaging (MRI) over Computerized Axial Tomography (CAT) in detecting head injuries 32-34. Cavum septi pellucidi, also known as the "fifth ventricle", is a normal anatomical variation occurring in as many as 0.73% of adults. Cavum septi pellucidi in a boxer has been considered a sign of pugilistic encephalopathy and in previous studies, as much as 18% have been found to show this sign on the CAT scan 35. The significance of cavum septi pellucidi is still difficult to interpret. Other frequent findings on the CAT scan are brain atrophy and ventricular dilation. Even with them, the CA T scan is still the study of choice in severe acute brain damage with the possibility of subdural hematoma, altered substantia alba and focal contusions. Although sometimes these lesions are not perceptible on a CAT scan and for better definition you need an MRI of the skull, since it provides a clear anatomic definition of the insult ruling out "lesions" seen on the CAT scan, ultimately they are concretely defined as artifacts on the MRI 36. The superiority of an MRI over a CAT scan is a result of several factors including a. multiple plan capacity to scan the images, b. absence of artifacts from adjacent bones and c. a high degree of contrast between the encephalon and cerebrospinal fluid (CSF) on TI imaging. With the MRI, the cerebral cortex is directIy visualized in a way impossible for a CAT scan. It allows for direct observation of a small hematoma between the encephalon and the skull.
Magnetic Resonance Spectroscopy (MRS) is a non-invasive method providing information on the chemical pathology of conditions affecting the central nervous system. Visible high peaks on the MRS are mainly derived from N-acetyl aspartate (NAA) and amino acids found almost exclusively with neurons and their processes on the adult encephalon. In a study, Davie et al 37. Compared 3 former professional boxers who developed Parkinson's syndrome, to 6 patients with idiopathic Parkinson's disease and 6 healthy. controls. The study showed a markedly reduced absolute concentration of N-acetyl aspartate on lenticular nuclei of former boxers when compared to Parkinson's patients and the control group. These findings suggest that trauma plays a role in the development of Parkinson's syndrome in some individuals diagnosed with idiopathic Parkinson's.
THERAPY
Treating chronic traumatic brain injury may be aimed at improving motor, cognitive, and psychiatric manifestations of this syndrome. Patients showing signs of Parkinson's may be treated with levodopa/ carbidopa or other anti-Parkinson's drugs. Selegilin has been used as a neuroprotective agent against boxer neurodegeneration 42 albeit its efficacy in chronic traumatic brain injury has yet to be established. Treating cognitive alterations in chronic traumatic brain injury is controversial. The use of anticholinergic agents (e.g. tacrine, donepezil) requires further research. Studies in limited cases suggest donepezil may be effective in treating chronic cognitive alterations in individual with sustained chronic traumatic brain injury 43. This benefit in boxer chronic traumatic brain injury, however, is still undetermined. Experience in treating boxers with behavioral alterations or other psychiatric disorders associated to traumatic brain injury is limited.
PREVENTION
Given the limited therapies available and their outcome, preventing traumatic brain injury is the main key. In 1983 the Consulting Panel on Brain Damage in Boxing of the American Medical Association 44 concluded that banning boxing and improvements recommended by medical and administrative standards are the most appropriate. For instance, in New York State, two physicians are required to stay on the ringside in all professional fights. Furthermore, in that state, in US amateur boxing, the ringside physician has the authority to enter the ring during a fight or between rounds and may terminate any boxing exposure to prevent severe physical damage. The appropriate neurological evaluation of a boxer sustaining multiple brain injuries is another very important safety measure.
The value of using a helmet as head protection against brain damage is controversia!. Although it does decrease the number of facial lacerations, it does not reduce the number of knock-outs. However, it could potentially reduce the strength of a 1 000 pound hit to 500 pounds 45. Reduced impact by the helmet and the development of chronic traumatic brain injury is unknown. A solution previously implemented was to decrease the weight of boxing gloves to 10 pounds for amateur boxers and 11 pounds for professional flghters, to possibly reduce the hit intensity. With this, however, the hit is less buffered with greater exposure to fractures or other musculoskeletal head and/or hand injuries. Thus, reducing the glove weight was not a solution. Another important issue in prevention is reducing the number of rounds and thus reduces the brain damage. The World Boxing Council acted accordingly by reducing the number of rounds in championship fights from 15 to 12 rounds. To date, no results have been scientifically confirmed.
Undoubtedly, the methods necessary to prevent traumatic brain injury are many, although further epidemiological and clinical research is required to determine the risk factors leading to dementia pugilistica. Hence, it is necessary to legislate the practice of this sports as recommended by world literature.
CONCLUSIONS
Dementia pugilistica is the result of chronic traumatic brain injury referred to as the neurological disorder due to repeated head injuries. About 20% of professional boxers show manifestations of chronic traumatic brain injury compared to amateur boxers where this incidence is lower because of less physical exposure due to head protection and the reduced number of rounds in fights as well as the stringent safety ruIes on the ring. Several risk factors to develop chronic traumatic brain injury are known. There is also a body of knowledge on the possible pathophysiological bases and pathological characteristics of chronic traumatic brain injury from brain biopsies where a similarity to Alzheimer's disease is found. The clinical picture involves neuropsychiatric disorders such as cognitive, behavioral, and thinking alterations as well as Parkinson's like motor alterations. Diagnosis is based on the history of exposure as a boxer, neuropsychiatric studies, an EEG, a CAT scan and MRI.
Preventing chronic traumatic brain injury in boxing is based on regular legislation of boxing with stringent medical and administrative rules, in addition to further research in this area to produce evidence on the main factors involved in dementia pugilistica.
Whatever degree of physical or cognitive disability occurs due to traumatic brain injury, perhaps the main prevention might be to assess a possible exclusion of contact sports.
REFERENCES
1. Mendez MF. The neuropsychiatric aspects ofboxing. Int J Psychiatry 1995;25:249-62. [ Links ]
2. La Cava G. Boxer's encephalopathy. J Sports Med Phys Fitness, 1963;3:87-92. [ Links ]
3. Report of the board of science and education working party on boxing. London. British Medical Association 1984. [ Links ]
4. Jordan BD, Jahre C, Hauser W A. CT of 338 active professional boxers. Radiology 1992;2:181-5. [ Links ]
5. Critchley M. Medical aspects of boxing, particular1y from aneurological standpoint. Br Med J 1957; 1 :357-62. [ Links ]
6. Jordan BD, Relkin NR, Raudin LD. Apoliprotein Ee4 associated with chronic traumatic brain injury in boxing. JAMA 1997; 278:136-40. [ Links ]
7. Katzman R, Galasko DR, Saitoht. Apolipoprotein e4 and head trauma: Synergistic or additive risk? Neurology 1996;46:889-92. [ Links ]
8. Nicoll J AR, Roberts GW, Graham DL. Apolpipoprotein Ee4 allele is associated with deposition of amyloid beta protein following head injury. Nat Med 1995; 1: 135-7. [ Links ]
9. Jordan BD, Kanick AB, Horwich MS. Apolipoprotein Ee4 and fatal cerebral amyloid angiopathy associated with dementia pugilistica. Ann Neurol 1995;38:698-9. [ Links ]
10. Martimer JA, French LR, Hutton JT. Head injury as a risk factor for Alzheimer's disease. Neurology 1985;35:264-7. [ Links ]
11. Merz Brown. Is boxing a risk factor for Alzheimer? JAMA 1989;261:2597-8. [ Links ]
12. Martland HS. Punch drunk. JAMA 1928;91:1103-7. [ Links ]
13. Roberts AH. Brain damage in boxers. A study of the prevalenceof traumatic encephalopathy among exprofessional boxers. Pitrnan, London 1969. [ Links ]
14. Guterman A, Smith RW. Neurological sequelae ofboxing. Sports Medicine. 1987;4:194-210. [ Links ]
15. Kaste M, Vilkki J, Sainis K, Kumme T, Katevuo K, Neurula H. Is chronic brain damage in boxing a hazard of the past? Lancet 1982;II: 1186-8. [ Links ]
16. Estwanik JJ, Boitano M, Ari N. Amateur boxing injuries at the 1981 and 1982 USAlABF national championships. Phys Sportsmed 1984; 12: 123-8. [ Links ]
17. Jordan BD, Campbell E. Acute boxing injuries among professional boxers in New York State: A two year survey. Med Sci Sports Exerc 1985; 17:212. [ Links ]
18. Moore M. The challenge of boxing ringing safety into the ring. Phys Sportsmed 1980;8:101-5. [ Links ]
19. Parkinson D. The biomechanics of concussion. Clin Neurosurg 1982;29: 131-45. [ Links ]
20. Corsellis JAN, Bruton CJ, Freeman-Browne C. The after math of boxing. Psychol Med 1973;3:270-303. [ Links ]
21. Corsellis JAN. Posttraumatic dementia in Alzheimer's disease. In: Jatzman R, Terry RD, Bick K, Eds. Senile dementia and related disorders. New York. Raven Press 1978. [ Links ]
22. PR Hof, C Bouras, l. Buée. Differential distribution of neurofibrillary tangles in the cerebral cortex of dementia pugilistica and Alzheimer's disease cases. Acta neuropathol 1992;85:23-30. [ Links ]
23. Roberts GW. Immunocytochemistry of neurofibrillary tangles in dementia pugilistica and Alzheimer's disease: evidence for common genesis. Lancet 1998;11:1456-8. [ Links ]
24. Tokuda T, Ikeda S. Re-examination of ex boxer's brains using immunohistochemistry with antibodies to amyloid 13- protein and tau protein. Acta Neuropathol 1991 ;82:280-5. [ Links ]
25. Mortimer JA, French LR, Hutton JT. Head injury as a risk factor for Alzheimer's disease. Neurology 1985;35:264-7. [ Links ]
26. Merz Brown. Is boxing a risk factor for Alzheimer's? JAMA 1989;261:2597-8. [ Links ]
27. Dale GE, Leigh PN, Luthert P. Neurofibrillary tangles in dementia pugilistica are ubiquitinated. J Neurol Neurosurg Psychiatry 1991;54: 116-8. [ Links ]
28. Uhl GR, McKinney M, Hedreen JC. Dementia pugilistica: loss of basal forebrain cholinergic neurons and cortical cholinergic markers. Ann Neurol 1982;12:99. [ Links ]
29. Butler RJ. Neuropsychological investigation of amateur boxers. Br J Sports Med 1994; 28:18790 [ Links ]
30. Jordan BD. Epidemiology of brain injury in boxing. In: Jordan BD, ed. Medical aspects of boxing. Boca Raton, FL: CRC Press 1993; 147-68. [ Links ]
31. Greg McLatchie; Neil Brooks. Clinical Neurological examination, neuropsychology, electroencephalography and computed tomographic head scanning in active amateur boxers. J Neurol Neurosurg Psychiatry 1987; 50:96-9. [ Links ]
32. Gandy SE, Snow RB, Zirnmerman RD, Deck MDF. Cranial nuclear imaging in head trauma. Ann Neurol 1984;16:254-7. [ Links ]
33. Han JS, Kaufman B, Alfidi RJ. Head trauma evaluated by magnetic resonance and computerized tomography: a comparison. Radiology 1984;150:71-7. [ Links ]
34. Y oung IR, Bydder GM, Hall AS. Extracerebral collections:recognition by NMR imaging. AJNR 1983;4:833-4. [ Links ]
35. Casson IR, Siegal O, Sham R, Campbell EA,. Brain damage in modem boxers. JAMA 1984;251:2663-7. [ Links ]
36. Barry DJ, Robert D, Zirnmerman. Computed tomography and magnetic resonance imaging comparisons in boxers. JAMA 1990; 263;1670-4. [ Links ]
37. CA, Davie, Z Pirtosek. Magnetic resonance spectroscopic studyofparkinsonism related to boxing . J Neurol Neurosurg Psychatry 1995;58:688-91. [ Links ]
38. Nicoll JAR, Roberts GW, Graham DI. Apolipoprotein Ee4 allele is associated with deposition ofamyloid beta protein following head injury. Nat Med 1995;1:135-7. [ Links ]
39. Mayeaux R, Ottoman R, Maestre G. Synergistic effects of traumatic head injury and apolipoprotein e4 in patientes with Alzheimer's disease. Neurology 1995;45:555-7. [ Links ]
40. Case records of the Massachusetts General Hospital. N Engl J Med 1999;340:1269-77. [ Links ]
41. Seliger G, Lichtman SW, Polsky T. The effect of apolipoprotein E on short-term recovery from head injury. Neurology 1997; 48: A 213. [ Links ]
42. Colosimo C, Albanese A. Boxer disqualified for taking selegiline. Lancet 1995;346:647. [ Links ]
43. Tavemi JP, Seliger G. Donepezil medicated memory improvement in traumatic brain injury during post acute rehabilitation. Brain Injury 1998;12:77-80. [ Links ]
44. Council on Scientific Affairs: Brain injury in boxing. JAMA 1983;249:254-7. [ Links ]
45. Ryan AJ. Eliminate boxing gloves. Phys Sportsmed 1983; 11:49. [ Links ]














