OPIOIDS AS NEW PSYCHOACTIVE SUBSTANCES
New psychoactive substances (NPSs) are misused compounds not controlled by the 1961 or 1971 Conventions on Narcotic Drugs. They are referred to as "new" because of their current market availability, not the date of their synthesis. NPSs are usually advertised in digital channels as "legal highs," "chemical reagents," or "designer drugs," frequently bought with cryptocurrencies and short-lived due to continued replacement by other synthetic analogs. Slight changes in the chemical structures of known addictive substances produce novel synthetic compounds which circumvent existing regulations. Some NPSs are "failed" medications, never marketed due to their adverse effects. Therefore, clinical research reports on humans do not exist or are very limited1.
According to the United Nations office on drugs and crime (UNODC), as of March 2023, 1185 individual NPSs had been reported in 141 countries. They include hallucinogens, dissociative anesthetics, sedatives/hypnotics, stimulants, synthetic cannabinoids, and 126 individual synthetic opioids (from 52 countries), which account for approximately 11% of the total2. In addition, synthetic opioids have increased from 14 in 2015 to 88 in 2020 and 126 in 2023. This paper reviews new psychoactive opioids (NPOs) and the challenges they pose to prevention and treatment (Fig. 1).
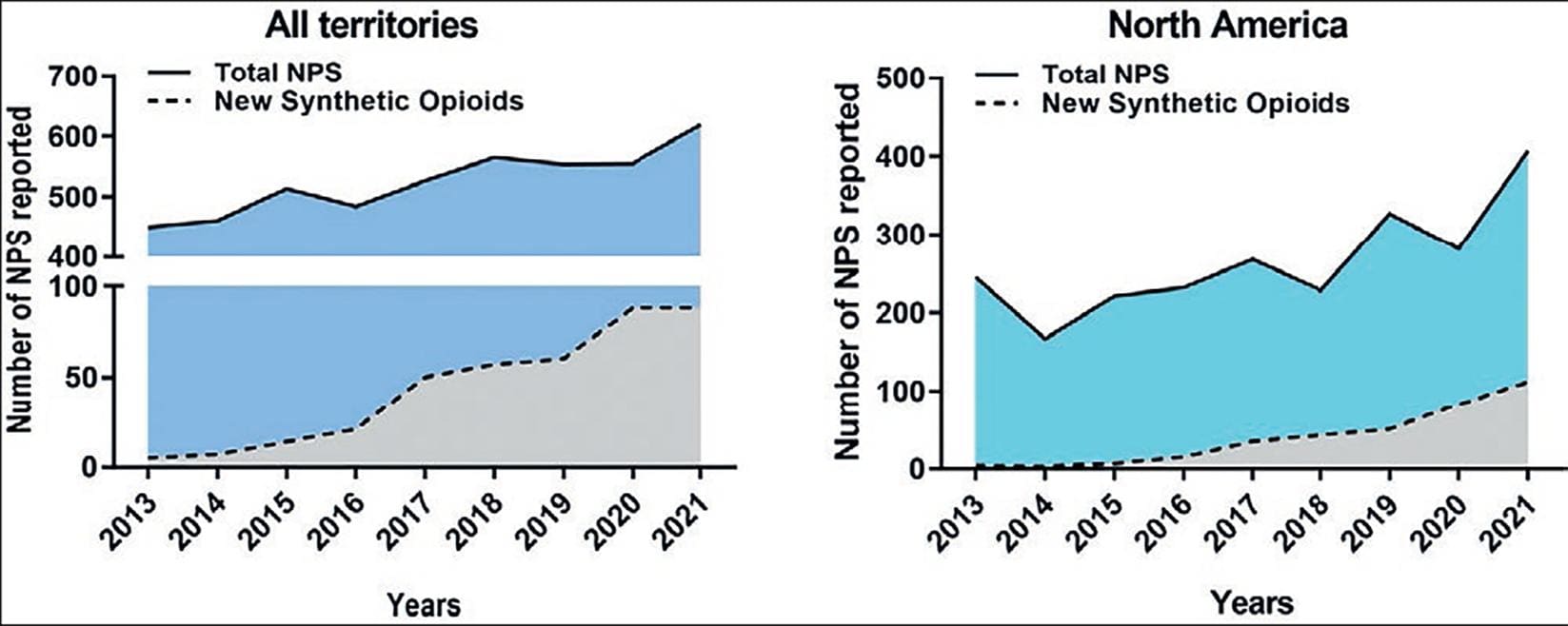
Figure 1. (A) New psychoactive substances and new synthetic opioids reported from 2013 to 2021 by UNODC in 141 reporting territories, and (B) North America (Mexico, United States, and Canada)2.
EFFECTS AND MECHANISM OF ACTION OF OPIOIDS
To understand the actions of NPOs, it is necessary to review the effects of morphine, the opiate prototype. Morphine is a natural compound found in the sap of unripe pods of the poppy plant Papaver somniferum. It is a five-ring compound with a phenanthrene nucleus, a furane ring, and a heterocycle ring with an amine (-NH2) group. Opiates include natural analgesics (e.g., morphine and codeine) and semisynthetic compounds with morphine-like chemical structure or effects. Heroin, oxycodone, hydromorphine (opioid receptor agonists), naloxone, and naltrexone (opioid receptor antagonists) are semisynthetic opiates. The term opioids is broader because it comprises opiates, endogenous peptides (e.g., enkephalins, endorphins, dynorphins), and compounds with chemical structures different from morphine but similar effects (reviewed in Cruz et al.3). Fentanyl and fentanyl derivatives are opioids, not opiates.
Morphine produces analgesia, euphoria, drowsiness, sedation, miosis, and cough suppression. At high doses, morphine inhibits the respiratory center in the brain stem, causing slow breathing and death. Other effects include decreased gastrointestinal secretions and motility, urinary retention, itching, and orthostatic hypotension. Morphine also decreases adrenocorticotropic hormone, corticotropin-releasing hormone, cortisol levels, and gonadotropin-releasing hormone secretion. Repeated use leads to tolerance development, dependence, neuroendocrine alterations, and immunosuppression (Fig. 2).
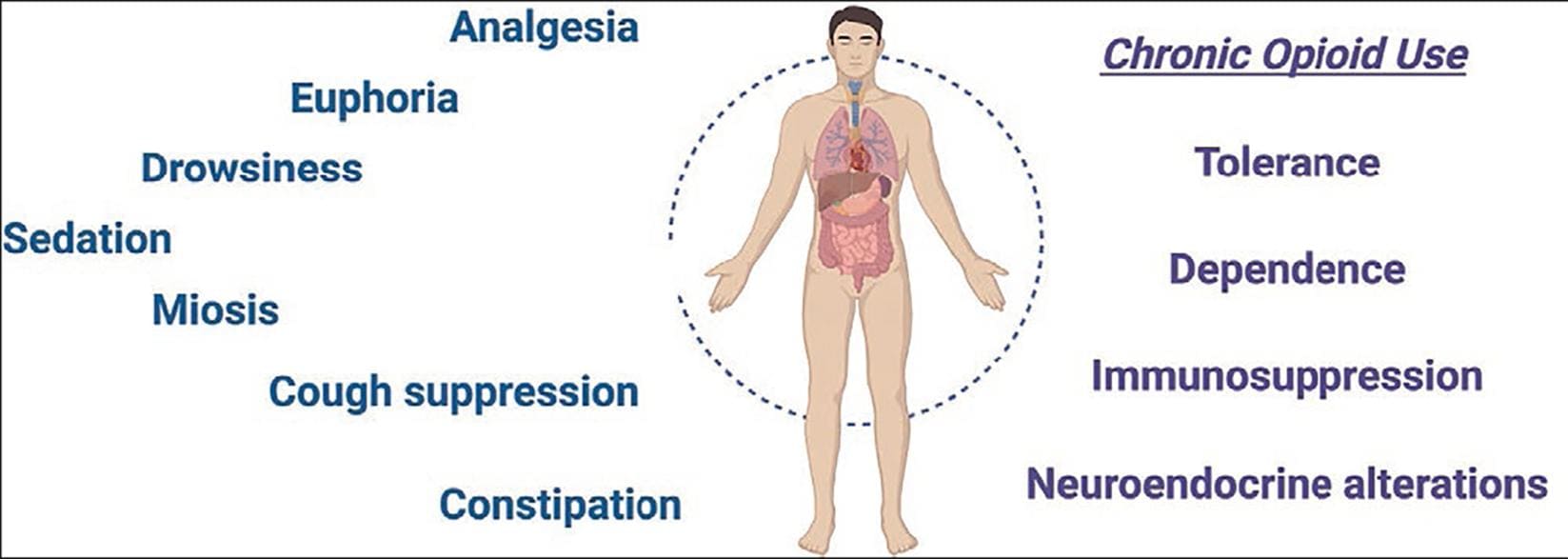
Figure 2. Main systemic effects produced by morphine and other opioid receptor agonists. Created with BioRender.
Complete tolerance can occur to morphine's analgesic effects. However, only partial tolerance develops to respiratory depression, pupil constriction, and constipation3.
Morphine acts on three classical opioid receptor subtypes: mu- (μ-) delta- (δ-), and kappa- (κ-) opioid receptors, also called MOR, DOR, and KOR, respectively. In addition, a fourth receptor with high homology was cloned, opioid receptor-like 1 (ORL-1) or nociceptin/orphanin FQ (N). ORL-1 evolved from the opioid receptor family; nociception is its endogenous ligand and has negligible affinity for the non-selective opioid receptor antagonist naloxone.
MOR mediates most of the clinically relevant actions of opioid receptor agonists in the central and peripheral nervous systems, and naloxone can block them at low nanomolar concentrations. When morphine binds to MOR, it causes the dissociation of the αi-GTP subunit from the βγ-subunit complex. The αi-subunit inhibits the adenylyl cyclase, thus decreasing the intracellular levels of cyclic adenosine monophosphate (cAMP). This prevents protein kinase A activation and the subsequent phosphorylation of the transcription factor cAMP responsive element binding protein, inhibiting the synthesis of proteins, including the endogenous opioids. In addition, the βγ -subunit complex increases the conductance of ATP-sensitive and inwardly rectifying potassium channels (KATP and GIRK, respectively) and decreases voltage-gated calcium channels (Cav) conductance. These effects result in cell hyperpolarization and decreased responsiveness4. The βγ complex has two additional effects: the activation of phospholipase C and mitogen-activated kinase cascades (Fig. 3. Reviewed in Carranza-Aguilar et al.5).
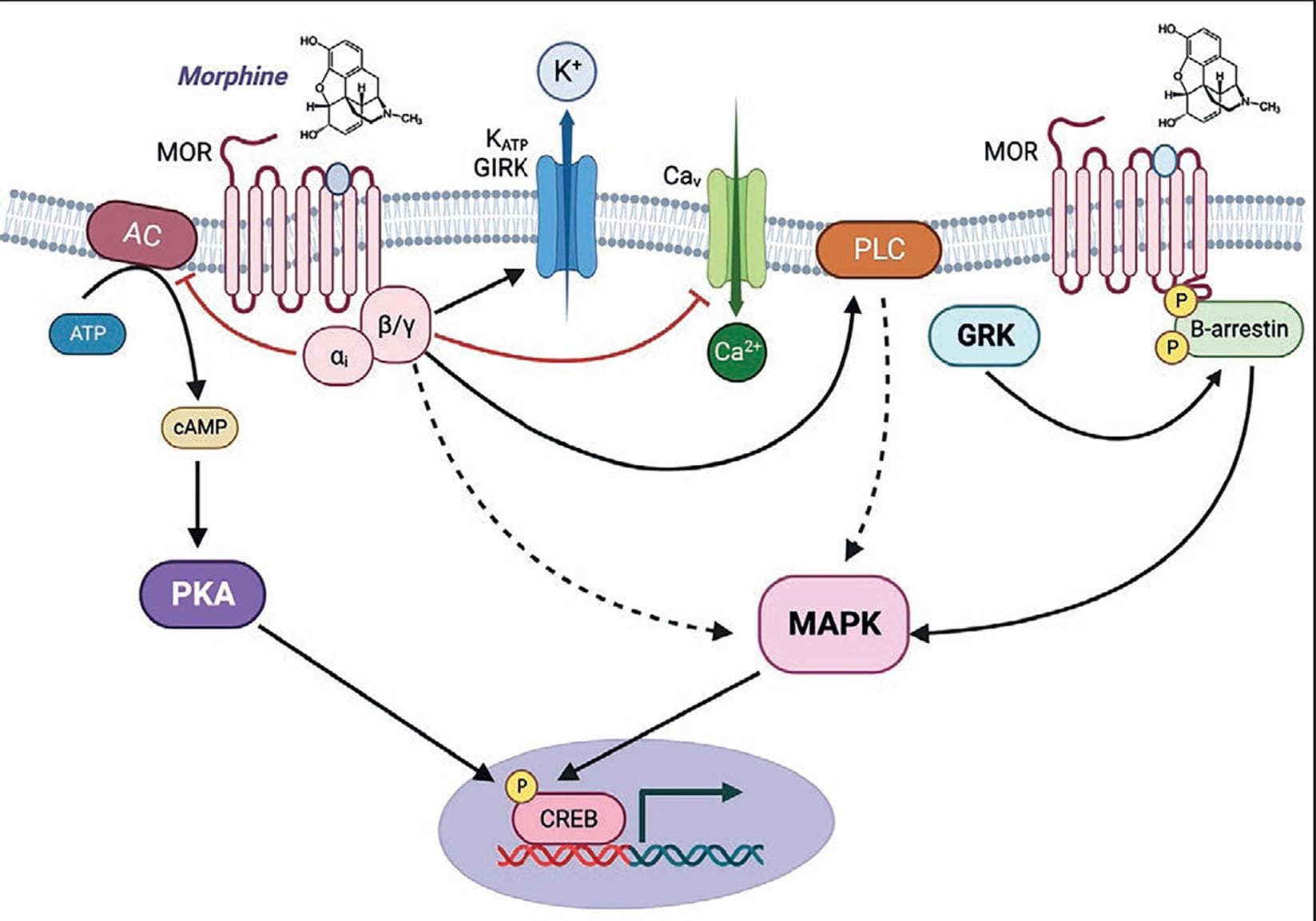
Figure 3. Mechanisms of action common to morphine and other opioid receptor agonists. AC: adenylyl cyclase; cAMP: cyclic adenosine monophosphate; PKA cAMP-dependent protein kinase; CREB: cAMP response element-binding protein; GIRK: G protein-coupled inwardly rectifying potassium channel; GRKs: G-protein-coupled receptor kinases. KATP: ATP-sensitive potassium channel. PLC: phospholipase C; MAPK: mitogen-activated protein kinase. MOR: -opioid receptor. MOR signaling ends with the phosphorylation of the active receptor by G protein receptor kinases (GRKs) and subsequent binding of β-arrestin, causing receptor desensitization, internalization, trafficking, and recycling. Created with BioRender.
THE ROLE OF NEW PSYCHOACTIVE OPIOIDS IN THE OPIOID CRISIS IN THE U.S.
Opioid misuse is a worldwide public health problem. In the U.S., drug overdose deaths have increased fivefold since 1999. In 2020, 75% of deaths involved an opioid, and from 2019 to 2020, synthetic opioid-related death rates increased by 56%6.
The opioid crisis is usually described as having three waves, although a fourth one is rising. The first wave was iatrogenic. It began in the late 1990s and was caused by opioid over-prescription, mainly of extended-release oxycodone (OxyContin®). The figures speak for themselves: U.S. pharmacies dispensed 76 million opioid prescriptions in 1991 compared to 219 million in 20117. Aggressive marketing programs under the pretense that prolonged opioid use for pain management rarely produced dependence contributed to an unprecedented increase in opioid use. In addition, pharmaceutical companies introduced formulations with high opioid concentrations, which increased the prevalence of opioid use disorders (OUD) and fatal overdoses. Sells of highly-concentrated prescription opioids skyrocketed in the black market when it became clear that OxyContin® pills could be crushed and injected to get a "high" like that produced by heroin. The second wave began around 2010 when a significant proportion of patients with chronic pain who had developed OUD switched to heroin. At that time, the pharmaceutical company that sold OxyContin® added a coating to the pills, making it impossible to crush and misuse. In addition, associations of physicians reformulated the existing guidelines for pain treatment, and the health authorities developed a National Digital Database to record the number of opioid prescriptions. The increased presence of heroin laced with fentanyl and fentanyl analogs triggered the third wave of the opioid crisis in 2013. Acetylfentanyl, furanyl-fentanyl, cyclopropylfentanyl, and other analogs began to appear in counterfeit pills or powdered heroin. These substances were subjected to control after their identification in forensic analyses. By the end of 2020, more than 30 fentanyl-related substances had been scheduled8.
The NPSs Discovery Program, an early warning system, has detected new drugs in the U.S. illicit markets since 2018. This program identified 137 NPSs from 2018 to 2022, 30.6% of which were synthetic opioids9. Fentanyl analogs and non-fentanyl synthetic opioids are now responsible for most fatal opioid overdoses in what some authors consider the fourth wave of the opioid crisis.10
CLASSES OF NEW PSYCHOACTIVE OPIOIDS
Synthetic opioids can be broadly divided into fentanyl analogs and non-fentanyl opioids. Fentanyl analogs account for 65% of the NPOs reported2. Some examples are carfentanil, butyrylfentanyl, acetylfentanyl, fluorofentanyl, bromofentanyl, and furanylfentanyl. Based on their chemical structure, fentanyl analogs pertain to the phenylpiperidine class of opioids characterized by an aromatic phenyl group attached to a piperidine group (Fig. 4). Examples of non-fentanyl NPOs include brorphine, etonitazene, and U-47700.
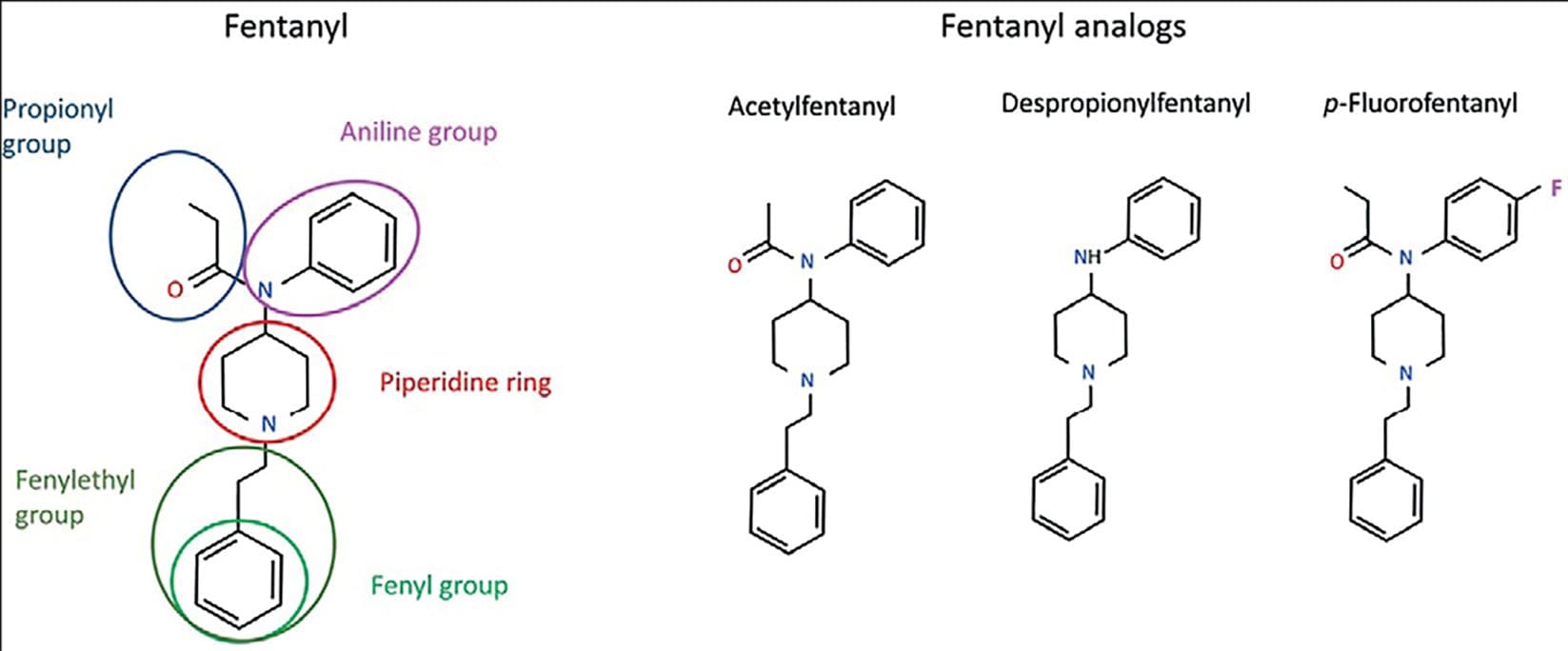
Figure 4. Chemical structure showing the regions that can be modified in the fentanyl molecule to produce new derivatives and examples of selected fentanyl-like drugs identified in seized samples.
Fentanyl analogs
Fentanyl
Fentanyl is a full MOR agonist, highly lipophilic, and 100 times more potent than morphine. Paul Janssen synthesized fentanyl in 1959, and the drug enforcement administration (DEA) approved it for human use in the U.S. in 1968. Since then, fentanyl has become a valuable therapeutic tool, given its potency, analgesic, and sedative effects. The early onset of fentanyl's action and its short half-life make this opioid particularly useful in brief surgical procedures as a common adjunct to anesthesia. Fentanyl is also an effective analgesic for patients with cancer or under palliative care. Pharmaceutical presentations of fentanyl include injectable solutions, dermal patches, nasal sprays, lollipops, and products for buccal and sublingual administrations8. However, high doses of fentanyl can produce muscle rigidity and adverse effects common to other MOR opioid agonists, including respiratory depression and dependence. Due to its therapeutic properties and dependence risk, fentanyl is a Schedule II narcotic according to the U.S. Controlled Substance Act of 1970. This category corresponds to drugs with a high abuse risk but accepted medical uses.
Medical and street fentanyl differ in several essential aspects. As a medication used for over 50 years in clinical settings, fentanyl is a safe and valuable therapeutic tool. The method to synthesize it is the same one patented by Janssen. Professional laboratories produce pharmaceutical formulations under controlled protocols, which adhere to high-quality control standards. This ensures that only fentanyl citrate, the soluble salt, is present in the medical products at the proper concentrations. In addition, trained personnel prescribe and administer medical fentanyl when needed.
On the other hand, illicit fentanyl formulations are synthesized in clandestine laboratories following different chemical pathways, depending on the precursors available. Others can be used if a specific substance is difficult to get. Moreover, precursors can be synthesized from pre-precursors with legal uses. Regardless of the method used, the synthesis and purification of street fentanyl are rudimentary, leaving chemical reagents and residues in the final product.
Because fentanyl and fentanyl derivatives are entirely made in laboratories, there is no need to cultivate the poppy plant and wait until harvest time. Furthermore, due to its high potency, low quantities of fentanyl, easy to conceal and transport, are enough to produce millions of doses. It has been estimated that 1 kg of fentanyl is enough to kill half a million people11. Assuming that most street doses are not lethal, the revenues of the drug are formidable.
There are many fentanyl derivatives. Three have medical uses and one is a veterinary drug (see below). The rest are not for human use, despite being sold as NPOs12. Fig. 4 shows fentanyl's chemical structure with the regions that can be modified and some fentanyl analogs. The next sections provide information of some of these substances.
Alfentanil, sufentanil, and remifentanil
These three clinically- used fentanyl derivatives have similar pharmacological profiles and are generally used as adjuncts to general anesthesia. However, they differ in their potency and pharmacokinetics. Alfentanil is the least potent compound, has a very short onset of action, and its effects last only 10-15 min. Therefore, it is helpful for short and ambulatory procedures but not as an analgesic. Sufentanil is 7-10 times more potent than fentanyl and is effective in patients with tolerance to opioids. It has recently been approved in the European Union and the U.S. for acute pain management in a 30-mg sublingual tablet presentation. Remifentanil is an ultra-short-acting opioid (onset of action in 1 min), and its effects dissipate rapidly (10 min) even after prolonged infusions.
Carfentanil
Carfentanil is 10,000 times more potent than morphine and is used to immobilize large animals and manage pain. Due to its veterinary use, it is frequently known as "elephant tranquilizer" or "drop dead." At present, carfentanil is used in science and nuclear medicine as a radiotracer ([11C]-carfentanil) for positron emission tomography imaging for studying μ-opioid receptors in the human brain13-15. The first detection of carfentanil in the illicit market occurred in 2017 as an adulterant to heroin, cocaine, and counterfeit prescribed drugs, significantly increasing overdose risk. Due to its high potency, multiple naloxone doses are usually required to counteract carfentanil's effects16.
Furanylfentanyl
Huang and collaborators synthesized furanylfentanyl in the 1980s as a potential analgesic. This substance is 50-100 times more potent than morphine. Many furanylfentanyl-involved intoxications and deaths have been documented since its appearance in the illegal market in 201517. Furanylfentanyl can be smoked or injected as a standalone product or mixed with other illicit drugs such as fentanyl, heroin, cocaine, oxycodone, or other NPOs. Furanylfentanyl's effects are not immediate, causing the users to increase the dose to achieve the desired effects. This practice can easily lead to overdoses. Of interest, 4-anilino-N-phenethylpiperidine (4-NPP) is both a furanylfentanyl metabolite and a precursor in the synthesis of fentanyl.
Acetylfentanyl
Acetylfentanyl (Fig. 4) appeared in the illicit market in 2013 and was associated with numerous overdose deaths on the U.S. East Coast. It is less potent than fentanyl but approximately ×15 more potent than morphine. As it occurs with furanylfentanyl, acetylfentanyl can be metabolized to 4-NPP18. In addition, there is an evidence that acetylfentanyl can also be used in electronic cigarettes and mixed with alcoholic beverages.
Butyrfentanyl
Butyrfentanyl is another fentanyl analog that appeared in the illicit market in 2015, causing a growing number of deaths related to its use. As a result, it was scheduled by the DEA in 201719.
Fluorofentanyl
This halogenated fentanyl analog was first identified in 2016 and has become more prevalent in postmortem samples. It has three isomers, ortho- (o-), meta -(m-), and para- (p-), according to the position of the fluor atom in the aniline group of the fentanyl molecule (Fig. 4). p-Fluorofentanyl is the most common isomer and has a similar potency to fentanyl but appears to be more lethal20. The toxicology information on p-fluorofentanyl is scant; however, from July 2020 to June 2021, nearly 65,000 overdose deaths involving this substance were reported by 43 jurisdictions in the U.S21. These deaths commonly involve concomitant use of illicit fentanyl, which complicates understanding the role of p-fluorofentanyl by itself. Table 1 summarizes basic information on selected fentanyl analogs.
Table 1. Basic information of representative fentanyl NPOs
| Compound | Potency | Findings in forensic studies in the last 5 years | First report as adulterant | Scheduling (year) |
|---|---|---|---|---|
| Fentanyl | ×50-100 | Of 543 opioid-related deaths in Ohio, in 2017, 63% involved fentanyl use42 | ~2006 | II (1970) |
| Carfentanil | ×10,000 | Carfentanil was involved in 35% of the opioid-related deaths in Ohio, in 201742 | 2017 | II (2018) |
| Furanylfentanyl | ×50-100 | Responsible for 7 fatal overdoses in Sweden43 | 2015 | I (2018) |
| Cocaine laced with furanylfentayl caused 44 non-fatal overdoses in 4 days in Canada44 | ||||
| Acetylfentanyl | ×15 | A study assessing fentanyl intoxication in 270 impaired-driving cases found fentanyl with acetylfentanyl45 | 2013 | I (2016) |
| Butyrfentanyl | ×7 | Two cases of fatal overdoses involved butyrfentanyl in Florida, United States; 201646 | 2015 | I (2017) |
| Fluorofentanyl | ~×100 | Fluorofentanyl was identified in 33% of 370 postmortem cases in Florida, from 10/2020 to 04/202147 | 2016 | I (2020) |
Non-fentanyl new psychoactive opioids
Many non-fentanyl analogs exist. Those presented here are some examples of the ones detected in heroin and other drug samples. Depending on their chemical structure, it is possible to distinguish several classes of non-fentanyl NPOs.
Benzimidazole derivatives
Brorphine belongs to a class of synthetic opioids like fentanyl but has a chemical group (benzimidazole) that prevents it from being regulated as a fentanyl-derivative (Fig. 5). Janssen synthesized brorphine in 1967. Like most NPOs, it is a full μ-opioid receptor agonist, more potent than morphine and similar to fentanyl. Brorphine emerged as a NPO in 2018, producing over 100 fatalities in 2020. It was advertised in unregulated markets as a fentanyl substitute, sold as a mixture known as "purple heroin" (due to the color added to the powder), or as counterfeit oxycodone pills22,23.
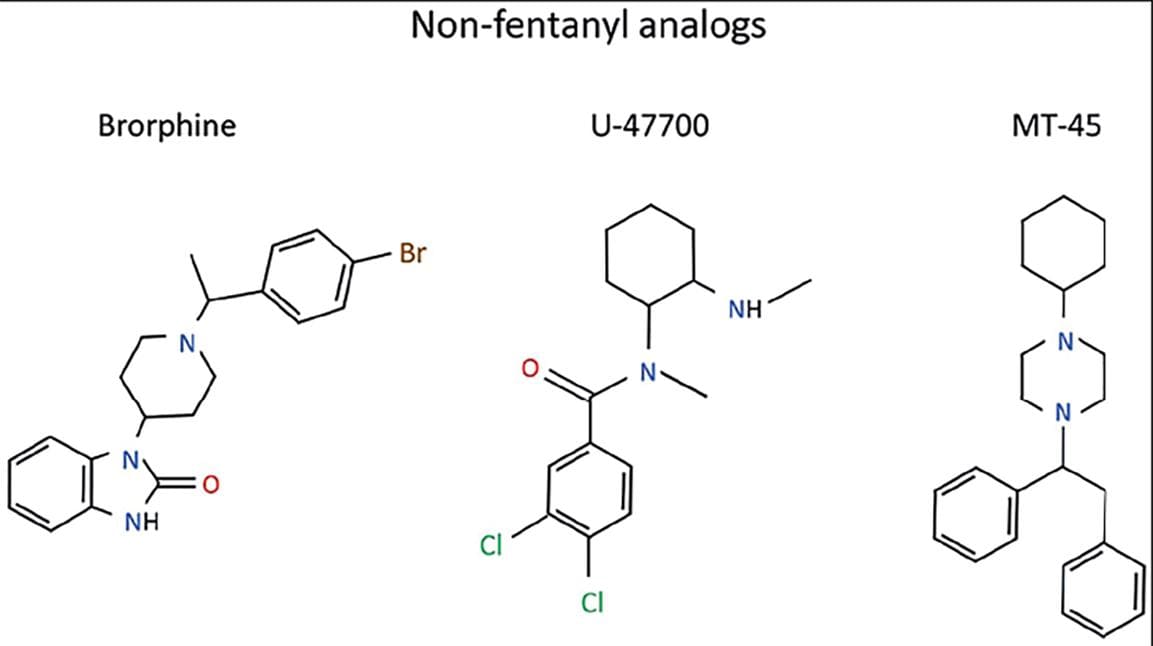
Figure 5. Chemical structure of representative non-fentanyl drugs. Brorphine is a benzimidazole derivative, and U-47700 is a member of the U-series compounds.
Other benzimidazole derivatives are aromatic hydrocarbons with benzene and imidazole groups fused, generically called nitazenes. The CIBA Swiss pharmaceutical company first synthesized etonitazene and related compounds in the 1950s as potential analgesics. However, these substances were not considered good candidates for clinical use due to safety concerns and lack of advantages over already available analgesics. The emergence of benzimidazole opioids in the illicit markets is very recent (in 2019). Several members of this group have been identified in seized samples, mainly in the U.S. Of them, etonitazene is 1000 times more potent than morphine, isotonitazine, ×500, protonitazene, ×200, and metonitazene, ×100. Their high potency (like fentanyl or higher) makes these compounds dangerous24. This led to a rapid regulation of etonitazene, metonitazene, isotonitazene, and etodesnitazene. However, there are about 30 additional available analogs25. The most recent report of the Center for forensic science research and education (CFSRE) in the U.S. detected protonitazene, N-pyrrolidine etonitazene, metonitazene, etodesnitazene, and isonitazene in biological samples and seized material, showing that these drugs are on the rise, contributing to recent fatal overdoses26-28.
U-47700 and related compounds (benzamide derivatives or U-series analogs)
U-47700, U-49900, U-44800, and U-51754 were synthesized in the 1970s by Upjohn laboratories (hence the U in their code name) while looking for new analgesics with fewer adverse effects than the existing opioids. From the chemical point of view, these substances pertain to the benzamide family, having a benzene ring linked to a carboxamide group (-C(=O)-NH2).
U-47700, also known as "pink," (Fig. 5) was synthesized in 1978 and detected in the streets in 2014. Like other group members, U-47700 produces sedation, euphoria, analgesia, pinpoint pupils, constipation, and all the adverse effects of morphine. U-47700 is a μ-opioid receptor agonist approximately 7.5 times more potent than morphine. It has a relatively rapid onset after oral administration and insufflation (15 min), and its effects last up to 7 h. Due to fatalities associated with U-47700, this drug became controlled in 2017. The same year, U-48800 emerged as a substitute for the scheduled U-47700. U-48800 was also synthesized in the 1970s and had similar efficacy and potency to U-47700. A closely analog, U-49900, appeared online for sale in 2016, advertised as a "research chemical." The information on this compound is scarce, but according to experiences shared in online drug forums, U49900 has a caustic odor, can cause smell loss, and is not a good analgesic29,30.
AH-7921 is another benzamide opioid analgesic developed in the 1970s by the Allen and Hanburys Limited Pharmaceutical Company (later bought by Glaxo). Although this compound is an analgesic as potent as morphine, it was not further developed because of its addiction liability. AH-7921 caused several fatal overdoses, usually combined with fentanyl analogs, and is now a Schedule I controlled substance.
MT-45
Like other NPOs, MT-45 was developed in the 1970s. It is chemically unrelated to other synthetic non-fentanyl opioids (Fig. 5). MT-45 has a similar potency to morphine and can produce hearing loss and dissociative-like effects like those produced by NMDA receptor antagonists. After the scheduling of MT-45, fluorinated derivatives appeared in the streets.
As with other misused substances, non-fentanyl NPOs can be combined. For example, in 2019, a solid gray product known as "gray death" was identified in the U.S. as a mixture of heroin, three fentanyl analogs, and U-4770031. Table 2 provides basic information on selected non-fentanyl NPOs.
Table 2. Basic information of representative non-fentanyl NPOs
| Compound | Synonyms | First Report | Potency | Scheduling (year) |
|---|---|---|---|---|
| Etonitazine | 2-[2-[(4-ethoxyphenyl)methyl]-5-nitrobenzimidazol-1-yl]-N,N-diethylethanamine | 2019 | ~×10 fentanyl | I (2021) |
| U-47700 | 3,4-dichloro-N-[1R,2R)-2-(dimethylamino) cyclohexyl]-N-methylbenzamide, "pinky, pink, U4" | 2014 | ~×7.5 morphine | I (2017) |
| Brorphine | 3-[1-[1-(4-bromophenyl)ethyl]piperidin-4-yl]-1H-benzimidazol-2-one | 2018 | ~fentanyl | I (2022) |
| MT-45 | 1-Cyclohexyl-4-(1,2-diphenylethyl) piperazine | ~morphine | I (2015) |
TRENDS IN NEW PSYCHOACTIVE OPIOIDS USE IN MEXICO
A few reports in the scientific literature provide a glimpse of NPSs use in Mexico (Table 3). A recent study assessing drug use in pregnant women found that 42% of the study participants consumed one or more psychoactive substances during pregnancy. Of them, 2.3% tested positive for NPSs, including norfentanyl, a fentanyl metabolite32.
Table 3. Evidence of fentanyl and other synthetic opioids consumption in Mexico
| Synthetic opioid | Region of study | Number of participants/Sample | Main findings | References |
|---|---|---|---|---|
| Fentanyl Nor-fentanyl | Pregnant women, Guadalajara, Mexico | (n = 300) | 42% of participants used one or more psychoactive substances during pregnancy 2.3% of the participants tested positive for NPS | 32 |
| Fentanyl | Northern Mexicans cities | Forty pharmacies | 25% of the pharmacies analyzed sold
counterfeit drugs 30% of the counterfeit samples contained fentanyl |
37 |
| Fentanyl | Fifteen Mexican cities | Wastewater | Evidence of fentanyl use in borderline cities; higher during weekends | 36 |
| Fentanyl | Tijuana | 89 drug residues | 93% of "China white" (powdered heroin) contained fentanyl | 33 |
Mexican cities near the U.S.-Mexico border have a high prevalence of drug use33. For example, there is an evidence that up to 54% of people who inject drugs (PWID) living in San Diego travel to Mexico to use drugs34,35 because they perceive easier access to cheaper and better-quality drugs.
Information on NPSs use also comes from a wastewater-based epidemiological study that analyzed samples in 15 Mexican cities and found evidence of fentanyl use in several borderline towns, with increased weekend consumption. According to this study, PWIDs prefer to travel to Mexico as they perceive easier access to cheaper and better-quality drugs. The cities chosen for this study reflected different levels of drug use nationwide36.
Another study conducted in borderline Mexican cities assessed the presence of fentanyl in the paraphernalia left by heroin users (drug wrappings, syringe plungers, or metal cookers), finding that 93% of the China white heroin samples contained fentanyl. Most drug users in this study reported no intended use of fentanyl, reflecting the danger of increased overdose risk when consuming fentanyl-laced drugs33.
On the other hand, counterfeit-prescribed drugs play an essential role in the opioid epidemic, posing an increasing risk of overdose, as synthetic opioids have higher potency and shorter life than prescription opioids. A recent study conducted in Northern Mexican cities evaluated counterfeit prescription drugs' availability and composition. The researchers demonstrated that ten out of 40 pharmacies sold counterfeit prescription drugs, easy to purchase as single pills and without a prescription, and that 30% contained fentanyl37. Despite these data, we lack statistics on drug-related fatalities due to the paucity of forensic and toxicological data.
CHALLENGES TO PREVENTION AND TREATMENT POSED BY NEW PSYCHOACTIVE OPIOIDS
The NPSs scene constantly evolves. Therefore, surveillance and monitoring programs are critical to keep up with the associated public health challenges. Some examples of monitoring programs are the European Monitoring Centre for drugs and drug addiction in Europe, the early warning advisory (EWA) program of the UNODC38, and the CFSRE in the US. The information they provide is necessary to prioritize NPSs for international review and eventual scheduling and regulation. It is imperative to implement regional drug testing and forensic services where they do not exist. In addition, laboratories must modify their current methodologies or develop new forensic and toxicological analytic methods to detect the emerging drugs. This can be challenging as data about NPSs emergence differ between regions and become rapidly outdated1.
The NPSs Discovery program and the Society of Forensics Toxicologist Designer Drugs Committee have established recommendations for NPSs detection, categorizing them into three tiers of analysis: Tier 1- strongly recommended (includes metonitazene, fluorofentanyl, brorphine, isotonitazene, and carfentanil); Tier 2- recommended, and Tier 3- consider testing. It is worth noting that substances in each tier constantly evolve39.
The proliferation of NPOs is a worldwide problem that requires multilateral approaches because these substances are available through the dark web, easy to conceal, and easy to deliver through regular or express mail services. Clinicians must consider that commonly available antidoping kits may not detect fentanyl analogs and other new synthetic opioids and stay alert to symptoms associated with opioid use, especially slow and shallow breathing, cyanosis, and miosis. In those cases, naloxone is the drug of choice to counteract opioid intoxication. Due to the high potency of fentanyl and other synthetic opioids, it may be necessary to administer several naloxone doses (or several nasal spray administrations where Narcan® is available), and more prolonged observation periods. Naloxone is an effective antidote without intrinsic activity that displaces opioid drugs from their receptors, effectively counteracting the life-threatening respiratory depression caused by heroin, fentanyl, and other NOPs1. Naloxone is internationally accepted to help opioid users recover from respiratory depression and has saved countless lives40.
CONCLUSION
Recommendations to avoid or decrease the number of opioid-related fatalities include:
– Develop and maintain surveillance programs for monitoring drug trends and rapid NPSs identification.
– Raise awareness about the risks associated with opioid use through public health alerts and evidence-based prevention programs.
– Implement drug checking services, syringe exchange programs, self-consumption services, and other harm reduction strategies for PWIDs (reviewed in Rafful and Magis-Rodríguez41).
– Offer medication-assisted programs for people with opioid use dependence.
– Make naloxone available to drug users and first respondents.











 nueva página del texto (beta)
nueva página del texto (beta)


