Servicios Personalizados
Revista
Articulo
Indicadores
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Salud mental
versión impresa ISSN 0185-3325
Salud Ment vol.34 no.1 México ene./feb. 2011
Artículo original
Effect of acupuncture treatment on depression: Correlation between psychological outcomes and salivary cortisol levels
Efecto del tratamiento de acunpuntura sobre depresión: un estudio de correlación sobre variables psicológicas y niveles de cortisol salivar
Roxana D. Vázquez,1 Laura González-Macías,2 Carlos Berlanga,3 Francisco J. Aedo4
1 Graduate and Research Section. ENMyH. National Polytechnic Institute.
2 Clinical Research Division. National Institute of Psychiatry.
3 Director of Clinical Research Division. National Institute of Psychiatry.
4 Latinamerican School of Integrative Medicine.
Corresponding:
Francisco J Aedo. M.D. MSc.
Profesor. Latinamerican School of Integrative Medicine.
Orion 1 1 7. Colonia Prado Churubusco, Coyoacán 04230, México, D.F.
Tel. / Fax. (55) 5582 1 792.
E-mail: aedo0770@yahoo.com.mx
Recibido: 2 de septiembre de 2010.
Aceptado: 18 de octubre de 2010.
Abstract
Introduction
There are growing scientific data that show the potential therapeutic benefit of treating depression with acupuncture. The most studied mechanisms of action of antidepressants, such as the monoamine oxidase inhibitors, tricyclic antidepressants or serotonine reuptake inhibitors, are their ability to enhance the synaptic availability or the binding of these monoamines to their respective receptors and their effect on adaptations within signal transduction pathways downstream from monoamine receptors. Life stressors or psycho-social events play a significant role in precipitating a first or second episode of major depression. Physiologically, stress activates the Hypothalamic-Pituitary-Adrenal (HPA) axis. Activation of the axis begins with the release of a corticotrophin-releasing factor (CRF), which stimulates the remainder of the cascade, successively prompting the release of adrenocorticotrophic hormone (ACTH) and cortisol. Multiple reports have related HPA axis hyperactivity, including CNS (i.e., corticotrophin-releasing factor), pituitary (i.e., adrenocorticotrophic hormone), and adrenal (i.e., cortisol) to major depression, and suicide behaviour. One of the resources of TCM for the treatment of depression is acupuncture, and it has been suggested as an alternative to antidepressants for its action on the brain monoaminergic systems. Up to now, there are a few examples of randomized and controlled clinical trials of the effect of acupuncture and electroacupuncture on major depression and we have obtained similar results when using acupuncture and electroacupuncture or conventional antidepressant drugs. Since the 1970's many reports have been done to explain the mechanism of action of acupuncture. Some studies performed in humans and animals studies had found an increment in the levels of 3-endorphin, ACTH and cortisol following low frequency electroacupuncture. The release of ACTH and cortisol suggests that electroacupuncture is acting on the HPA axis and through this mechanism could have a modulatory effect on the stress system and depression. The influence of acupuncture on different neurotransmitter systems like 3-endorphin itself or monoamines, like noradrenaline and serotonine, can also mediate effects of acupuncture on mood and behavior.
The aim of this study was to establish the effect of a low frequency electroacupuncture point formula on the clinical improvement of depressed patients and its relation with changes on salivary cortisol.
Material and methods
Subjects: 42 patients, recruitment and Study Population, at a Universitary Primary Care clinic and randomly divided into control (sham acupuncture) or case group (real acupuncture).
Intervention: Low frequency electroacupuncture point formula Main Outcome Measures: Clinical score in the Carroll Scale for Depression and psychiatric Symptoms Check List (SCL-90). Salivary cortisol
Results
The formula used in this study showed a major effect on the reduction of the depressive symptomatology of patients studied compared to the control group.
Conclusions
To our knowledge, this is the very first report on acupuncture treatment that evaluates depression symptoms and its evolution using the Carroll rating scale. Effect over depressive symptomatology was higher in the real acupuncture group than in the sham acupuncture group. Taking all data together, the formula used in this study showed a major effect on the reduction of the depressive symptomatology and Cortisol levels of patients studied compared to the sham control group.
Key words: Acupuncture, depression and salivary cortisol.
Resumen
Antecedentes
La medicina moderna describe la depresión como una enfermedad mental, que se caracteriza por al menos dos semanas continuas de presentar alguno de estos síntomas: labilidad emocional, pérdida del interés en actividades que resultaban placenteras, sentimientos de culpa y aburrimiento, nivel de energía notablemente disminuido, cambio en el patrón de sueño y en el apetito, pérdida de la concentración, agitación psicomotora, pensamientos relacionados con la muerte, sentimiento de desesperanza, irritabilidad y decremento de la libido, afectando las diversas áreas de funcionamiento: sociales, laborales e interpersonales. Investigaciones recientes han encontrado que los trastorno afectivos muestran un beneficio terapéutico en el tratamiento con acupuntura. Se sabe que el estrés de los eventos de la vida pone a las personas en alto riesgo de presentar un cuadro depresivo. Psicológicamente el estrés activa el eje hipotalámico— adrenal-pituitario (HPA); esta activación del eje comienza con la relación del factor liberador de corticotropina, el cual estimula el resto de la cascada, promoviendo sucesivamente la producción de hormona adrenocorticotrópica.
Eje hipotálamo-hipófisis-adrenal. La activación de este eje comienza con la liberación del Factor liberador de corticotropina (FLC), que estimula una cascada que sucesivamente incrementa la liberación de la hormona adrenocorticotrópica (ACTH) y el cortisol. Múltiples reportes han relacionado la hiperactividad de este eje con la depresión mayor y la conducta de suicidio. Se ha sugerido que el hipercortisolismo puede ser un factor relevante en la patogénesis de la depresión.
Otros hallazgos que refuerzan la hipótesis anterior son el incremento de cortisol y los pulsos secretores de ACTH, así como los niveles elevados de CRF en el fluido corticoespinal, y un incremento de neuronas secretoras de CRF en la región límbica del cerebro con una disminución del número de receptores de CRH en la corteza frontal, y alteraciones en la prueba de supresión con dexametasona en pacientes deprimidos.
Dentro de la perspectiva de la acupuntura, la depresión es tratada con el método de nutrir al corazón y calmar la mente, regulando la energía y la sangre. Por lo anterior, se sugiere la acupuntura como una alternativa para la sintomatología de la depresión, ya que por su acción en el sistema monoaminérgico en el cerebro actúa como antidepresivo. Algunos estudios han reportado el efecto de la acupuntura y la electroacupuntura en la depresión mayor, mostrando resultados similares al uso de las drogas antidepresivas. También la acupuntura y la electroacupuntura han demostrado en algunos estudios, tanto en humanos como en animales, el incremento de los niveles de p-endorfinas, ACTH y cortisol. La relación del ACTH y el cortisol sugiere que la electroacupuntura activa el eje HPA y a través de este mecanismo se puede modular el efecto en el sistema de la depresión y el estrés, así como la influencia de la acupuntura en los diferentes neurotransmi-sores del sistema, como las p-endorfinas, monoaminas, noradrenalina y serotonina.
Objetivo
Establecer el efecto de la baja frecuencia de electroacupuntura en los puntos clínicos adecuados para manejar la depresión en relación con el cortisol en la saliva.
Material y métodos
Cuarenta y dos pacientes de la población general, divididos en grupo control y grupo experimental, siguiendo un diseño doble ciego, haciendo una intervención de baja frecuencia de electroacupuntura, en puntos adecuados y en puntos placebo, midiendo el cortisol en saliva y utilizando la escala de Carroll para medir sintomatología depresiva y la escala de síntomas psiquiátricos (SCL - 90).
Resultados
La fórmula utilizada en el estudio mostró un mayor efecto en la reducción de la sintomatología depresiva en los pacientes del grupo experimental que en los pacientes pertenecientes al grupo control. Estos resultados fueron observados hasta la sexta semana de tratamiento. La fórmula utilizada en este estudio mostró una disminución en los niveles de cortisol en los pacientes del grupo control.
Conclusiones
Desde nuestro punto de vista, éste es el primer reporte del tratamiento acupuntural que evalúa la sintomatología depresiva usando la escala de Carrol. El efecto sobre la sintomatología depresiva fué mayor en el grupo de acupuntura real que en el de acupuntura ficticia. Consideramos este efecto una respuesta parcial porque no hubo al menos una reducción de 50% de la sintomatología depresiva, la que se pudiera convertir en una respuesta completa si los pacientes fueran tratados por mayor tiempo o con otros esquemas acupunturales de tratamiento. Tomando en conjunto todos los datos, la formula usada en este estudio mostró un mayor efecto en la reducción de la sintomatología depresiva y en los niveles de cortisol en el grupo de los pacientes estudiados comparado con el grupo de los pacientes control.
Palabras clave: Acupuntura, depresión y cortisol en saliva.
INTRODUCTION
With a lifetime prevalence of 10% to 25% in women and 5% to 12% in men, major depressive disorder has become one of the leading causes of disability in the world.1 Modern medicine describes depression as a mental disease characterized for at least two weeks of symptoms like: dysphoric mood, loss of interest or pleasure, changes in sleep patterns and appetite, guilty or worrying feelings, diminished energy level, lose of concentration, psychomotor agitation or retardation, thoughts related to suicide, feelings of hopelessness, feelings of worthlessness, irritability, and decreased libido, with impairment in social, occupational, or other important areas of functioning that are not due to a substance, general medical condition, or bereavement.1 The most supported theory of depression surrounds the central fact that there is a deficiency of norepinephrine or serotonine in the synapse between neurons. The most studied mechanisms of action of antidepressants, such as the monoamine oxidase inhibitors, tricyclic antidepressants or serotonine reuptake inhibitors, are their ability to enhance the synaptic availability or the binding of these monoamines to their respective receptors1,2 and their effect on adaptations within signal transduction pathways downstream from monoamine receptors.3 At a psychological level, although a causal relationship between stressful life events and depression cannot be concluded, many studies have shown that some type of relationship might exist. Stressful life events put people at higher risks for depression, and life stressors or psychosocial events play a significant role in precipitating a first or second episode of major depression.4
Physiologically, stress activates the hypothalamic-pituitary-adrenal (HPA) axis. Activation of the axis begins with the release of corticotrophin-releasing factor (CRF), which stimulates the remainder of the cascade, successively prompting the release of adrenocorticotrophic hormone (ACTH) and cortisol.4 Multiple reports have related HPA axis hyperactivity, including CNS (i.e., corticotrophin-releasing factor), pituitary (i.e., adrenocorticotrophic hormone), and adrenal (i.e., cortisol) to major depression and suicide behaviour.4 It has been suggested that hyper-cortisolism may be a relevant factor in the pathogenesis of depressive disorder.5 Some other findings that reinforce this hypothesis are an increase in cortisol and ACTH secretory pulses, elevated levels of CRF in corticoespinal fluid, an increase of CRF-secreting neurons in limbic brain regions with diminished number of binding sites for CRH in frontal cortex, and alterations in dexametasone suppression test in depressed patients.4,5 Many antidepressants also show significant effects on synthesis, release, or response to CRH.2
One of the resources of TCM for the treatment of depression is acupuncture, and it has been suggested as an alternative to antidepressants for its action on the brain monoaminergic systems.6,7 Up to now, there are a few examples of randomized and controlled clinical trials of the effect of acupuncture and electroacupuncture on major depression. These trials have shown similar results when using acupuncture and electroacupuncture or conventional antidepressant drugs.8,9 Similar effects to psychotherapy have also been observed.10 Clinical studies on the effects of electroacupuncture at hormonal levels in major depression are very scarce. Dhar reported a reduction in thyroid hormonal levels in depressed patients treated with acupuncture.6 Also acupuncture has shown a blunted stress response measured by salivary cortisol levels in premature infants following ophthalmologic examination for retinopathy of prematurity.11 Other authors have found lower levels of cortisol during surgery, when acupuncture was combined with conventional anesthesia.12,13 Since the 1970's many reports have been done to explain the mechanism of action of the analgesic effect of acupuncture.14 It has been established that electroacupuncture at different frequencies lead to the stimulation of different brain nucleus and the release of different neuropeptides.14 Nowadays it is known that low frequency electroacupuncture (4Hz) leads to the activation of the anterior arcuate hypothalamic nucleus with a rise of proopiomelanocortine (POMC), a precursor of hormones like adrenocorticotrophic hormone (ACTH) and (3-endorphin.15 Furthermore, some studies performed in humans and animals studies have found an increment in the levels of (3-endorphin, ACTH and cortisol following low frequency electroacupuncture.16 The release of ACTH and cortisol suggests that electroacupuncture is acting on the HPA axis and through this mechanism could have a modulatory effect on the stress system and depression. Furthermore, the influence of acupuncture on different neurotransmitter systems like (3-endorphin itself or monoamines, like noradrenaline and serotonine, can also mediate effects of acupuncture on mood and behavior.17,18
The aim of this study was to establish the effect of low frequency electro-acupuncture on the clinical improvement of depressed patients and its relationship with changes on salivary cortisol.19
MATERIAL AND METHODS
Recruitment and study population
The study was carried out from August 2003 to March 2004. The study design was a controlled, double-blind, sham versus real acupuncture clinical trial. The patients were recruited at a universitary primary care clinic and randomly divided into control (sham acupuncture) or case group (real acupuncture). The inclusion criteria were: diagnosis of major depressive episode according to DSM-IV, a score in the Carroll rating scale for depression above 18, and age above 18 years old. Exclusion criteria were: suicidal tendency, organic brain syndrome, another major psychiatric disease, concomitant medication with antidepressants, psychotropic drugs including reserpine, severe diseases, substance abuse, and pregnancy or lactancy. All patients were informed about the aims of the study and an informed consent was obtained. The trial protocol was examined and approved before the start of the study by an ethics committee.
Procedures and measures
Before treatment, saliva samples were collected, psychological tests performed, and clinical history registered. The main outcome measure was the improvement in the Carroll rating scale for depression. Saliva samples were collected only in those patients that arrived on time to the clinical setting (between 7:30 and 8:00 a.m.). The salivary cortisol samples were stored at -70° until used. The temperament and character inventory (TCI) and the SCL-90 psychiatric rating scale were also evaluated.
The Carroll Rating Scale for Depression is an adaptation of the Hamilton rating scale. It has the advantage of being a good self-rating scale to establishing the severity of symptoms.20-22 We compared the ratings of the Carroll Scale before, during, and after treatment. The TCI is an instrument which describes personality within a psychobiological model20,23 and accounts for dimensions of both temperament and character. The temperament dimensions are: novelty seeking, harm avoidance and reward dependence. Novelty seeking is defined as the tendency to respond actively to novel stimuli leading to pursuit of rewards and escape from punishment. Harm avoidance is the tendency toward an inhibitory response to signals of aversive stimuli that lead to avoidance of punishment and non-reward. Reward dependence is the tendency for a positive response to signals of reward to maintain or resist behavior extinction. The character dimensions are self-directedness, cooperativeness and self-transcendence.
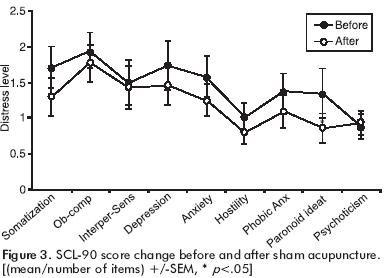
The definition of self-directedness refers to self-determination, or the ability of an individual to control and adapt behaviour to fit the situation in accord with individually chosen goals and values. Cooperativeness was formulated to account for individual differences in identification with and acceptance of other people. Self-transcendence which is associated to spirituality, refers to identification with everything conceived as essential and consequential parts of a unified whole.20,24 The TCI was measured at the beginning of the study. We compared the results of TCI with the Mexican23 and original standardizations.20 Although the Mexican and original standardization of the TCI test had proved to have no significant difference, we decided to compare our results with both of them to analyze any probable difference between our samples and standardizations. The SCL-90 is a self reported clinical rating scale focused toward the symptomatic behavior of psychiatric outpatients. The primary symptom dimensions measured by the SCL-90 are: somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. We compared the ratings of SCL-90 before and after treatment. Cortisol concentration was measured by ELISA using a kit from R&D System (Minneapolis, MN) and a MRX-microplate ELISA reader from Dynex (Kentucky, VA). The intra-assay precision was obtained with 10 samples and showed a good correlation (r2 = 0.945).
Intervention
Treatment was given by a medical doctor, acupuncture specialist. Acupuncture points selection was based on the TCM. Points used for the real acupuncture group were: left Shen Men, right Shen Shu, right Xin Shu, left Nei Guan, left San Yin Jiao, and bilateral Tai yang. All points were stimulated with low frequency electroacupuncture(4Hz), for 30 minutes twice a week, for six weeks. Intensity was graded up to the patient's threshold. Points used for the Sham acupuncture group were located as following: One point located by tracing an horizontal line that goes from the supraorbital border to the occipital and another vertical line from the anterior portion of the tragus where they join. Another point over the trapezoid bone, proximal to the articulation with the second metacarpal bone, and another over the back of the proximal epiphysis of the first metatarsal bone.
Statistical analysis
SPSS was used for data analysis. Student's t test, Mann Whitney U test, and Chi squared were used for establishing group differences depending on the variable. Mann Whitney U test was used to evaluate the differences in the Carroll rating scale of depression from day 0 up to week 6 and between groups. The Carroll intention to treat analysis, and changes in SCL-90 before and after treatment were made using Wilcoxon T test.
RESULTS
During the time of the study 42 patients were recruited, 23 for real acupuncture group and 19 for sham group. The baseline status of demographic, personality, severity of depression, and salivary cortisol between real and sham acupuncture groups are summarized in Table 1. These data show that both treatment groups were essentially similar at baseline. Figure 1 shows that real acupuncture has a higher effect on Carroll rating scale than sham after four weeks of treatment. This difference was statistically significant after six weeks of treatment. The Wilcoxon T test was carried out to evaluate the impact of the intervention on patients scores on the SCL-90. It showed a statistically significant decrease in somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism in the real acupuncture group after six weeks of treatment. The sham group shows a statistically significant decrease in paranoid ideation, a tendency to decrease in somatization, and no statistically significant decrease in obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, and phobic anxiety (figures 2 and 3 and table 2). Comparing the TCI scores of both groups with the Mexican and original standarization of the test we found our patients significantly higher in harm avoidance (p<0.001) and self-trascendence (p<0.05) and lower in self-directedness (p<0.001). Intention to treat analysis shows a statistically significant larger effect on real acupuncture (mean difference: -10.44) than on sham acupuncture (mean difference: -3.01) in the Carroll rating scale (table 2). We found a normalization of salivary cortisol levels in the real acupuncture group compared with a sample salivary cortisol of healthy people after six weeks of treatment (table 2).




DISCUSSION
Acupuncture shows a wide variety of response with diverse points and ways of stimulation, offering a large possibility of depression treatments. Within this variety, some studies on the effects of different electric frequencies applied to acupuncture points help us to estimate the effects of acupuncture, particularly on the endocrine and nervous systems. These effects might have potential roles in the treatment of certain diseases like depression. Therefore it is possible to design a formula which includes points that according to TCM are used in depression treatment, employing low frequency electric stimulation on them. Patients of this study, clinically presenting the depression diagnostic, had their evolution and treatment evaluated with Carroll's scale. To our knowledge, this is the very first report on acupuncture treatment that evaluates depression symptoms and its evolution using the Carroll rating scale. Personality evolution by TCI showed characteristical features of depressive patients, which reinforced the depression diagnostic.21 Effect over depressive symptomatology was higher in the real acupuncture group than in the sham acupuncture group. We consider this effect as a partial response because there was not at least a 50% reduction on depressive symptomatology, which might become a full response if patients were treated for longer times or with another acupuncture scheme.
Beyond this effect, the group of patients treated with real acupuncture showed a significant reduction in all the dimensions of the psychiatric symptomatology measured by the SCL-90. In contrast, the sham acupuncture group showed only a reduction in paranoid ideation. Although the real acupuncture group had a decrease on salivary cortisol levels, the sham group was not different from the healthy control group before the study. This result could reflect a limitation in our study, because the sham group samples used to compare with the healthy control group could not reflect the effect of sham acupuncture in all the sample. We think it is recommendable for future studies to obtain samples at different hours of the day since the early morning peak levels of cortisol in depressed patients are marginally raised while the afternoon levels are elevated approximately two-fold;22 therefore we might not be observing a significant decrease of these levels.
Taking all data together, the formula used in this study showed a major effect on the reduction of the depressive symptomatology and cortisol levels of patients studied compared to the sham control group. This result was found until the sixth week or twelve sessions of treatment.
REFERENCES
1. More DJ, Bona JR. Depression and dysthymia. Med Clin North Am 2001;85:3. [ Links ]
2. Shelton RC. Cellular mechanisms in the vulnerability to depression and response to antidepressants. Psychiatr Clin North Am 2000;23:4. [ Links ]
3. Krystal JH, D'Souza DC, Sanacora G, Goddard AW et al. Current perspectives on the pathophysiology of schizophrenia, depression, and anxiety disorders. Med Clin North Am 2001;85:3. [ Links ]
4. Kaye J, Morton J, Bowcutt M, Maupin D. Stress, depression, and psy-choneuroimmunology. J Neurosci Nurs 2000;32:2-93. [ Links ]
5. Sher L. Life events cortisol, and depression. Psychother Psychosom 2003;72:289-90. [ Links ]
6. Dhar HL, Vsanti T. Endogenous depression, thyroid cunction and acupuncture. Indian J Physiol Pharmacol 2001;45(1):125-6. [ Links ]
7. Han JS. Electroacupunture: An alternative to antidepressants for treating affective diseases? Intern J Neuroscience 1986;29:79-92. [ Links ]
8. Roschke J, Wolf C, Muller MJ, Wagner P et al. The benefit from whole body acupuncture in major depression. J Affect Disord 2000;57:73-81. [ Links ]
9. Luo HC, Jia YK, Zhan L. Electroacupuncture vs. amytriptyline in the treatment of depresive states. J Tradit Chin Med 1985;5:3-8. [ Links ]
10. Allen JB, Schnyer RN, Hitt SK. The efficacy of acupuncture in the treatment of major depression in women. Psychol Sci 1998;9:397-401. [ Links ]
11. Schwartz L, Bauchner H, Blocleer R, Jorgensen K et al. Salivary cortisol as an indicator of stress in premature infants: The effect of electric stimulation of acupuncture meridians in blunting this response. Med Acu-punct 1998;10:2. [ Links ]
12. Yang QG, Hang YN, Sun DJ. Effect of combined drug-acupuncture anesthesia on hypothalamo-pituitary-adrenocortical axis response and glucose metabolism in open-heart surgery patients. Zhongguo Zhong Xi Yi Jie He ZaZhi 2001;21(10):729-731. [ Links ]
13. Zhu W, Xu Z. Alterations of plasma beta-EP and cortisol contents in thyroidectomy under acupuncture anesthesia and acupuncture anesthesia combined with tetrahydropalmatine. Zhen Ci Yan Jiu 1996;21(1):15-17. [ Links ]
14. Ulett GA, Han S, Han JS. Electroacupuncture: Mechanisms and clinical application. Biol Psychiatry 1998;44:129-38. [ Links ]
15. Han JS. Acupuncture: Neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci 2003;26(1):17-22. [ Links ]
16. Leong RJ, Chernow. The effects of acupuncture on operative pain and the hormonal responses to stress. International Anesthesiol Clin 1988;26(3):213-7. [ Links ]
17. Sher L. The role of the endogenous opioid system in the effect of acupuncture on mood and behavior: Theoretical and practical considerations. Am J Acupunct 1996;24(4):285-90. [ Links ]
18. Pomeranz B. Clinical acupuncture. Springer: Scientific Basis; 2001. [ Links ]
19. Bhagwagar Z, Hafizi S, Cowen P. Increase in concentration of walking salivary cortisol in recovered patients with depression. Am J Psychiatry 2003;160:1890-1. [ Links ]
20. Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatry 1993;50:975-90. [ Links ]
21. Berlanga C, Cortes J, Joachim B. Adaptación y validación de la Escala de Depresión de Carroll en español. Salud Mental 1991;15(4):36-40. [ Links ]
22. Carroll BJ, Feinberg M, Smouse P, Rawson SG et al. The Carroll Rating Scale for Depression I. Development, reliability and validation. Br J Psychiatry 1981;(138):194-200. [ Links ]
23. Sánchez de Carmona M, Páez F, López J, Nicolini H. Translation and reliability of temperament and character inventory. Salud Mental 1996;(19):5-9. [ Links ]
24. Flaws B, Lake J. Depression. Chinese medical psychiatry. Second ed. Blue Poppy Press; 2001. [ Links ]














