A 70-year-old hypertensive man with a triple coronary bypass surgery and isolated supracoronary ascending aorta replacement 4 years ago was submitted for a routine computed tomography as a control of a post-surgery periaortic hematoma. It revealed a pseudoaneurysm in the aortic root close to the right coronary sinus (Figs. 1A-C) surrounded by the periaortic hematoma and an aortic aneurysm in the distal ascending aorta. Echocardiography showed an anechoic image parallel to the ascending aorta not present in the previous studies with a mild aortic regurgitation and without any other finding. After careful Heart Team evaluation, the patient was finally taken for a redo surgery. Before performing the median esternotomy, the right femoral artery and vein were exposed in case after the esternotomy had to start cardiopulmonary bypass for myocardial damage. The saphenous vein of the right leg was harvested. After the sternum was open with oscillating saw, a great fibrosis was observed. The previous bypass of the left internal mammary artery (LIMA) to the anterior descending coronary artery (ADCA) was partially injured without hemodynamic instability. The pseudoaneurysm was big extending throughout the right atrium, so extracorporeal circulation (ECC) was performed through the femoral vein and aortic arch. Aortic clamping was performed with three clamps due to the enormous fibrosis due to the previous use of biological glue. The myocardial protection was performed with crystalloid through antegrade and retrograde cardioplegia. After the opening of the tube and the pseudoaneurysm, a 25 mm dehiscence of the previous suture between the tube and the aortic root was observed (Fig. 2). The corrective surgery consisted of myocardial revascularization with saphenous bypass to marginal obtuse and posterior interventricular coronary arteries and reconstruction of LIMA bypass to ADCA, removal of the previous tube and cleaning of contents and capsule of the pseudoaneurysm and replacement of the previous tube with a new 30 mm Dacron tube with double proximal suture and simple distal suture to aortic hemiarch, with a circulatory arrest of 39 min at 25°C of temperature, maintaining direct cerebral perfusion through the innominate arterial trunk and the carotid artery. The clamp and ECC times were 202 and 289 min, respectively. The post-operative evolution was without cardiac events until the 7th day when it was complicated by bronchoaspiration and digestive bleeding, and the patient finally died.
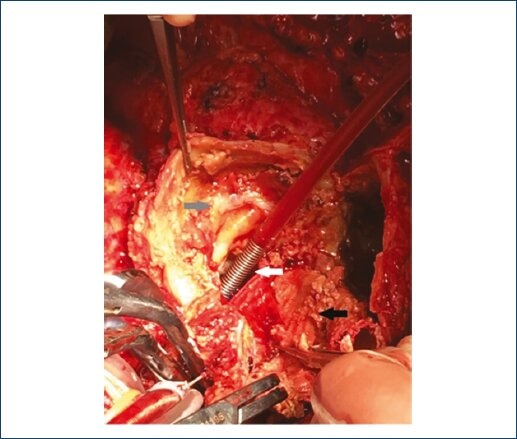
Figure 1 Surgery: white arrow: origin of pseudoaneurysm - dehiscence of 25 mm; black arrow: previous Dacron tube; gray arrow: capsule of pseudoaneurysm.

Figure 2 A-C: Aortic computed tomography (MPR LVOT, aortic root and ascending aorta, and 3DVR image) showing aortic pseudoaneurysm of the aortic root closed to the right coronary sinus.
Pseudoaneurysms of the thoracic aorta are an infrequent pathology. They result in transmural disruption of the aortic wall with the leak surrounded by mediastinal structures. Usually, they are secondary to the previous cardiac surgery, and the mechanisms implicated include poor anastomotic technique or an intrinsic aortic pathology; other causes reported are trauma and infections1,2. Surgical repair is the conventional treatment and mortality can reach 30%2. Favorable outcome has been associated with an appropriate surgical planning, adequate myocardial and cerebral protection, and a careful perioperative care. Percutaneous closure has also been reported with excellent outcome and must be considered, especially in high-risk patients2. In our patient, pseudoaneurysm was an incidental finding and this highlights the relevance of the careful and periodical follow-up of aortic patients using imaging techniques.











 nueva página del texto (beta)
nueva página del texto (beta)


