Artículos de revisión
The time of COVID-19: Clinical approaches and research within 2 months of arriving in Mexico
Tiempos de COVID-19: aproximaciones clínicas e investigaciones en dos meses desde su llegada en México
-
Publication dates-
Nov-Dec , 2020
July 30, 2021
- Article in PDF
- Article in XML
- Automatic translation
- Send this article by e-mail
- Share this article +
Abstract
By the end of 2019, a peculiar epidemic appeared in China; it was of the flu-type and revealed a lethal zoonosis caused by a beta coronavirus. In this study, we review the history of this new pandemic starting from its origin; we describe how COVID-19 spread its symptoms, especially the neurological ones, and the investigations currently underway.
Key words:
COVID-19, SARS-CoV-2, Symptoms, Diagnostic tests, Clinical trials
Introduction
By the end of 2019 in Wuhan, pneumonia of unknown etiology emerged. A new kind of betacoronavirus was identified when only two beta-coronaviruses were associated with respiratory syndromes in humans: Middle East Respiratory Syndrome Coronavirus (MERS-CoV) and Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV). The new virus was called SARS-CoV-2 by the International Committee of Virus Taxonomy. However, significant differences were found in transmission, pathogenesis, and clinical presentation between the new virus and the other SARS-CoV.
The surge of a new strain
The attendance to the Chinese Spring Festival implied the rapid mobilization of infected persons. The first five studied patients presented high fever and dry cough and four developed respiratory distress. Subsequently, a study in 137 patients concluded that middle-aged and elderly subjects with comorbidities have a poorer prognosis1. Next, angiotensin-converting enzyme-2 (ACE2) was identified as a SARS-CoV-2 receptor. ACE2 expression has been found in kidneys, intestines, gallbladder, nervous system, and placenta. In lungs, the target organ, it was much lower. On the other hand, ACE2 was strongly expressed in proximal tubules. Thirty-six of 536 patients presented acute renal failure 20 days after the onset, even though baseline creatinine levels were normal2.
-
1Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei ProvinceChin Med J, 2020
-
2Single-cell RNA sequencing data suggest a role for angiotensin-converting enzyme 2 in kidney impairment in patients infected with 2019-nCoVChin Med J, 2020
Clinical manifestations
Mainly respiratory, a dry cough accompanied by fever and mild constitutional symptoms is present in the first phase of the viral response (stage I). Then, shortness of breath without or with hypoxia corresponds to the moderate phase or pulmonary involvement, when patients develop viral pneumonia and when an abnormal chest computed tomography (CT) scan can be useful for rapid diagnosis to optimize management. A 3-stage classification and establishment of a standardized nomenclature were recently proposed for reporting the disease and orienting therapeutic interventions. Indeed, in stage II, the host’s inflammatory response increases until it reaches hyper inflammation in stage III with acute respiratory distress syndrome, systemic inflammatory response syndrome, and cardiac failure accompanied by the peak of pro-inflammatory cytokines, troponin, and NT-proBNP elevation. At this time, corticoid or immunomodulatory treatments can be beneficial3.
-
3COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposalJ Heart Lung Transplant, 2020
SARS-CoV-2 can affect other systems and cause abdominal pain, diarrhea, vomit, anorexia, acute renal failure, and a series of symptoms considered as neurological: dizziness, headache, consciousness impairment, acute cerebrovascular disease, ataxia, seizures, peripheral nervous system damage consisting of oculomotor palsy, the frequent anosmia/ageusia, other neuropathies, and also myalgias. In the mild phase of coronavirus disease (COVID)-19, an interplay between pro-inflammatory cytokines and chemokine release, increased endothelial damage, and potential sepsis induces coagulopathy development. It is known that the cytokine storm, macrophage activation, leukocyte adhesion molecule overexpression, together with the marked expression of ACE2 in the vascular endothelium, makes it a clear target of the disease. Therefore, COVID-patients are at risk of thrombogenesis due to both biochemical hypercoagulable state and direct vascular damage. A major neurological manifestation is ischemic stroke involving large vessels, often in multiple vascular territories and associated with elevated D-dimer, ferritin, anticardiolipin, and phospholipid antibodies4.
-
4COVID-19: a global threat to the nervous systemAnn Neurol, 2020
The mechanism of neuroinvasion has not been elucidated, though it could be due to a direct infection by SARS-CoV-2 as part of acute toxic encephalitis or by axonal transport through the olfactory system. The presence of viral particles in olfactory epithelium has been related to anosmia, an initial symptom that can persist until the moderate phase. The most severe phase of hyper inflammation threats the integrity of the blood-brain barrier. Toll-like receptors activation in microglia and astrocytes may explain the association with encephalitis, encephalomyelitis, acute necrotizing encephalopathy, meningitis, transverse myelitis, and acute cerebellar inflammation. Furthermore, post-infectious and immune mediate neurological complications are described, including Guillain-Barré syndrome and its variants that usually appear in the moderate and severe phases and some rare cases of acute disseminated encephalomyelitis-like encephalomyelitis4.
-
4COVID-19: a global threat to the nervous systemAnn Neurol, 2020
SARS-CoV-2 was isolated in cerebrospinal fluid from two patients with meningoencephalitis but not in nasal swabbing. One of them underwent severe disorder of consciousness; the other presented seizures. Previously, pediatric cases with Kawasaki-type vasculitis have been reported in New York. The first case, a 6-month infant had fever, tachycardia, tachypnea, irritability, conjunctivitis, and cracked lips. On day 5, the infant exhibited maculopapular exanthema and edema in limbs. Diagnosed with Kawasaki disease (KD) and immunoglobulin therapy was initiated. Eight pediatric English patients with KD showed shock signs; one died after ischemic strokes, and seven exhibited right heart ventricular failure. These latter improved after Immunoglobulin therapy and antibiotic treatment5.
-
5Hyperinflammatory shock in children during COVID-19 pandemicLancet, 2020
The arrival of the pandemic in Mexico
The first case of COVID-19 in Mexico, a 35-year-old male subject returning from Bergamo, Italy, was confirmed on February 28, while an increase in the number of cases in Western Europe was evident. Subsequently, preventive measures were taken such as avoiding physical contact and massive events (Table 1). On March 24, 405 cases were confirmed and phase 2 implemented with homeschooling and home-office during the quarantine (Fig. 1). At the beginning of April, a sharp rise in the contagion curve took place, but it was until April 21 that phase 3 of the pandemic was declared so as 857 deaths (Fig. 2).
Table 1
Control and prevention interventions of COVID-19 in different scenarios11
Control and prevention interventions of COVID-19 in different scenarios11
| Scenarios | 1. Viral import Dozens of cases | 2.-Community dispersion Hundreds of cases | 3.-Epidemic Thousands of cases |
| Greeting between people | No restriction | No kiss, no hug | No kiss, no hug |
| Closed public spaces (theaters, stadiums, cinemas, etc.) | Not necessary | Suspension of events before outbreaks | Suspension of events before outbreaks |
| Open public spaces (malls, parks, beaches) | Not necessary | Suspension of events before outbreaks | Suspension of events before outbreaks |
| Schools, high schools and universities | Dissemination of preventive messages | School filter | Suspension of classes in schools during active outbreak |
| Workplaces | Dissemination of preventive messages | Sanitary filter | Suspension of work activities in workplaces during active outbreak |
Thumbnail
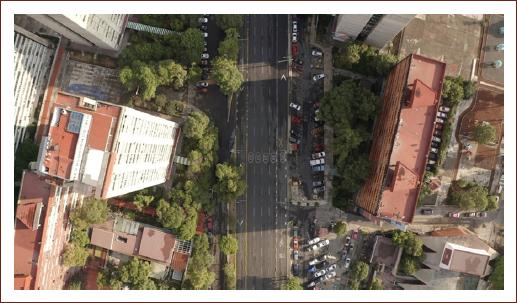
Figure 1
Empty avenue in Mexico City during April 2020 contingency. Photo bequeathed by DRONERO.MX.
Empty avenue in Mexico City during April 2020 contingency. Photo bequeathed by DRONERO.MX.
Thumbnail
Figure 2
Global death curves starting after the 6th death. Record as far as May 12, 2020 in ciencias.unam.mx/lansbiodyt/contacto with permission.
Global death curves starting after the 6th death. Record as far as May 12, 2020 in ciencias.unam.mx/lansbiodyt/contacto with permission.
Current research (Table 2)
After sequencing genetic material of SARS-CoV-2 (RNA), the first RT-polymerase chain reaction (PCR) diagnostic tests were developed. It has a sensitivity range of 56%-83% and specificity of 95%. The presence of the virus in aerosols and surfaces was then studied. SARS-CoV-2 remains in aerosols for 3 h and 8 h in copper; it is not found in carton after 24 h, but it is more stable on stainless steel for 48 h and on plastic with a viability of 72 h6. After PCR diagnostic test, serological tests were settled. A French laboratory developed a fast one called NG-Test IgG-IgM COVID-19 All-in-One that detects and differentiates antibodies against SARS-CoV-2 in blood. This test was carried out in 101 patients with COVID-19 and rendered a positive result in 95% on day 157.
-
6Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1N Engl J Med, 2020
-
7Rapid determination of SARS-CoV-2 antibodies using a bedside, point-of-care, serological testEmerg Microbes Infect, 2020
Table 2
Relevant ongoing research in March and April 2020
Relevant ongoing research in March and April 2020
| Type of study | Sample size | References | |
|---|---|---|---|
| NG-Test IgM-IgG COVID All-in-One detects specific antibodies anti-SARS-CoV-2 of IgG and IgM types in blood, serum, or plasma, producing results in 15 min. Positive outcome from day of infection to day 15 (p = 0.001) | Development of serologic test | 101 patients | Dortet et al. 20207 |
| Lansbiodyt Laboratory at the University of Mexico (UNAM) develops a biomarker that binds to SARS-CoV-2 virus and emits a quantifiable fluorescent signal at low cost. Project UNAM-INDRE-001 | Diagnostic test | 40 patients. On hold until financing is available | UNAM 202012 |
| Hydroxychloroquine and azithromycin as treatment for COVID-19 patients. It reduces viral load in PCR assay in nasopharyngeal swabbing (p < 0.001) | Non-randomized clinical trial | 36 patients | Gautret et al. 20208 |
| Countries with BCG vaccine as part of their individual policy show reduction in morbidity and mortality in patients with COVID-19 (p = 0.0001, and p = 0.05, respectively) | Epidemiologic study in cases and controls | 175 countries | Ozdemir et al. 202013 |
| Antiparasitic Ivermectin reduces the viral load in Vero cells infected with SARS-CoV-2 assayed by RT-PCR |
|
10 simulations | Caly et al. 20209 |
| Transplant of mesenchymal stem cells ACE2 reduces inflammation in patients with pneumonia caused by COVID-19 (p < 0.05) | Clinical trial | 10 patients | Leng et al. 202010 |
| Patients administered Remdesivir show a 2-point clinical improvement on a 1-6 scale after 10 days, with viral load reduction | Randomized clinical trial (pilot study) | 237 patients | Wang et al. 202014 |
| Patients treated with 200 mL of plasma from convalescent patients of COVID-19 show significant clinical, biochemical, and radiologic improvement | Open trial | 10 patients | Duan et al. 202015 |
| IgG and IgM antibodies target receptor S binding dominion (S-RBD) of SARS-CoV-2 and select it as humoral immunity target to become the aim for the development of vaccines | Pre-clinical phase and Phase 1 | 12 patients | Ni et al. 202016 |
In Mexico, the laboratory Lansbiodyt at the UNAM University is developing a biomarker detecting magnetic pearls that bind to the RNA of SARS-CoV-2 virus and send a fluorescent signal measured with a versatile biomolecule sensor. This method can detect a small viral load and is currently under validation.
Research on the control of hypoxic complications led to a clinical study in France on Arenicola marina, given that hemoglobin from this marine worm can transport 40 times more oxygen than the human one and is compatible with all human blood groups. The company Hemarina intends to use this hemoglobin for treating COVID-19. The study began in 10 patients with severe COVID-19 and on ventilators, but on April 19, the trial was stopped by the French Security Agency of Medicaments. In this same country, a study using hydroxychloroquine administered with azithromycin was carried out in 36 COVID-subjects when admitted to hospital. It was an open clinical trial. Main criticisms on this research are the risk of QT lengthening in the electrocardiogram and the low level of evidence, though the outcome was rather promising8.
-
8Hydroxychloroquine and azithromycin as a treatment of COVID-19:results of an open-label non-randomized clinical trialInt J Antimicrob Agents, 2020
Another therapeutic possibility is ivermectin, an antiparasitic with potent antiviral activity toward HIV and dengue. In a study in Vero/hSLAM cells infected with SARS-CoV-2, a 5 mM of ivermectin treatment showed after 24 h, that viral RNA was reduced by 93% in the supernatant. At 72 h, no remnant could be detected9. However, the dose utilized in Vero cells is 35 times higher than the Cmax allowed in human plasma after oral administration of the approved dose of ivermectin. At present, there is still no evidence of the efficacy of this drug in treating patients with COVID-19.
-
9The FDA approved drug Ivermectin inhibits the replication of SARS-CoV-2in vitroAntiviral Res, 2020
In the UK, RECOVERY, a randomized controlled trial, announced preliminary results in 2104 patients that showed that dexamethasone reduced significantly the 28-day mortality rate with the greatest benefit among those patients requiring mechanical ventilation but also in patients who only received oxygen therapy.
Among other therapeutic options, mesenchymal stem cells are expected to control the exacerbated immune response exhibited by patients. After cell transplantation, ten patients improved significantly in 2-4 days, PCR levels were low, also inflammatory cytokines diminished and chest CT showed a reduction in lung infiltration on the 9th day10. Meanwhile, an epidemiologic study in 175 countries shows a significant reduction in morbidity and mortality from COVID-19 in countries with BCG vaccine as part of their individual policy13.
-
10Transplantation of ACE2-mesenchymal stem cells improves the outcome of patients with COVID-19 pneumoniaAging Dis, 2020
-
13Is BCG vaccination effecting the spread and severity of COVID-19?Allergy, 2020
Another study in 10 severely ill COVID-19 patients explored the administration of plasma from recovered patients. This procedure significantly improved symptomatology and viral load15.
-
15Effectiveness of convalescent plasma therapy in severe COVID-19 patientsProc Natl Acad Sci USA, 2020
Vaccine research has been undertaken in different countries, reaching relatively advanced stages such as the recently published clinical trial with AD5-nCOV. One hundred eight healthy individuals received low (0.5 mL), medium (1.0 mL), or high (1.5 mL) doses of Ad5 vectored COVID-19 vaccine; 83% in low and medium doses and 75% in high doses reported mild or moderate adverse reactions consisting of pain in the injection site, fever, fatigue, headache, and myalgia. ELISA and neutralizing antibodies increased significantly from day 14 and specific T-cell response was rapidly reached17.
-
17Safety, tolerability, and immunogenicity of a recombinant adenovirus Type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trialLancet, 2020
In Mexico, ten patients with COVID-19 were participating in a clinical study to test the efficacy of remdesivir. On May 12, 9 out of 10 patients had been discharged and the antiviral clearly showed significant shortening in the course of the disease.
Conclusion
Similarly to COVID-19, research to fight the mortal agent will take quite a while. This pandemic has shown that we are facing a virus capable of disrupting global economy in a few months and draws attention to human fragility as was experienced in the big epidemics of antiquity, Middle ages, or the more recent Spanish Flu. Within a vicious circle, the economic and health repercussions slow down research progress at the risk of having to live the effects of SARS-CoV-2 for a long time. The whole world awaits the teachings of mass testing and the arrival of a vaccine. Furthermore, neurological manifestations that could be classified as early and systemic, neuroinvasion, and post-infectious immune-mediated have very diverse presentations and mechanisms that remain to be clarified.
References
-
1Liu K, Fang YY, Deng Y, Liu W, Wang MF, Ma JP, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J. 2020;133:1025-31. Links
-
2Deng YY, Zheng Y, Cai GY, Chen XM, Hong Q. Single-cell RNA sequencing data suggest a role for angiotensin-converting enzyme 2 in kidney impairment in patients infected with 2019-nCoV. Chin Med J. 2020;133:1129-31. Links
-
3Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states:a clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020;39:405-7. Links
-
4Koralnik IJ, Tyler KL. COVID-19:a global threat to the nervous system. Ann Neurol. 2020;88:1-11. Links
-
5Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020;395:1607-8. Links
-
6Van Doremalen N, Bushmarker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564-67. Links
-
7Dortet L, Emeraud C, Vauloup-Fellous C, Khecharem M, Ronat JB, Fortineau N, et al. Rapid determination of SARS-CoV-2 antibodies using a bedside, point-of-care, serological test. Emerg Microbes Infect. 2020;24:1-32. Links
-
8Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19:results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;2020:105949. Links
-
9Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA approved drug Ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020;178:104787. Links
-
10Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han Q, et al. Transplantation of ACE2-mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11:216-28. Links
-
11Secretaría de Salud. COVID-19 Comunicado Técnico Diario. Lunes 9 de marzo de 2020. Available at:https://www.gob.mx/cms/uploads/attachment/file/540170/COVID-19_-_Comunicado_Tecnico_Diario_2020.03.09.pdf Links
-
12Desarrollan en la UNAM biosensor para detección rápida de COVID-19. Boletín UNAM-DGCS-343/2020. Accessed March 17, 2020. Available at https://www.dgcs.unam.mx/boletin/bdboletin/2020_343.html. Links
-
13Ozdemir C, Kucuksezer UC, Tamay ZU. Is BCG vaccination effecting the spread and severity of COVID-19? Allergy. 2020;75:1824-7. Links
-
14Wang Y, Zhang D, Du G, Du R, Zhao J, Jin, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395:1569-78. Links
-
15Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Natl Acad Sci USA. 2020;117:9490-96. Links
-
16Ni L, Ye F, Cheng ML, Feng Y, Deng, YQ, et al. Detection of SARS-CoV-2-specific humoral and cellular immunity in COVID-19 convalescent individuals. Immunity. 2020;52:971-77. Links
-
17Zhu FC, Li YH, Guan XH, Hou LH, Wang WJ, Li JX, et al. Safety, tolerability, and immunogenicity of a recombinant adenovirus Type-5 vectored COVID-19 vaccine:a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020;395:1845-54. Links