Introduction
The different pathophysiological mechanisms that describe the behavior of metabolic surgery are not well-defined yet, but they are continuously being documented. There are two basic pillars that explain the functioning of this kind of surgery. First of all, the weight loss would reduce the insulin resistance of the peripheral tissue. Secondly, the gastrointestinal endocrine disruption, with hormones being synthesized in the digestive tract causing important changes of the behavior of glands - such as pancreas - and peripheral tissue1-3.
This second reason, at the same time, is based in two principal theories, the Foregut and the Hindgut theory. Both theories take into consideration the pass of the alimentary bolus through different sections of the digestive tube, which activates hormonal routes with favorable and unfavorable effects for the glycemic homeostasis4. The main hormones involved are called incretines, a numerous group that includes glucose-dependent insulinotropic polypeptide (GIP), glucagon-like peptide (GLP)-1, and ghrelin among other substances5,6.
The Hindgut theory is also known as the incretinic theory. It suggests that the early pass of the alimentary bolus as a result of a surgical procedure could explain the control of type 2 Diabetes Mellitus (T2DM). This early pass through the distal small bowel would stimulate the release of hormones such as GLP-1 or peptide tyrosine tyrosine7,8. That way, it would boost the insulin discharge, increasing its sensibility, and decreasing the beta cells apoptosis9.
In contrast, the anti-incretin effect is the cornerstone of the Foregut Theory. This opposite theory was based on the pass of nutrients through the proximal small bowel. The result is the release of different hormones. The anti-incretinic response buffers the previously cited incretinic effect. It produces a decrease in the discharge of insulin, decrease in the proliferation of beta cells and inhibition of the action of insulin, to prevent hypoglycemia10-12.
While a balanced and coordinated production of incretin and anti-incretin hormones is necessary to keep normal levels of glucose, a poor anti-incretin production may not compensate the effect of the incretins, resulting in hyperinsulinemia, hypoglycemia, and beta cells proliferation13.
On the other hand, a change toward the excessive production of the anti-incretin hormones would cause an insulin resistance, decrease in the insulin secretion and the beta cell depletion; all of them features of the T2DM10.
The purpose of this report is the study of the specific role of the ileum. We designed a new experimental surgical model. The use of non-obese healthy Wistar rats was pursued to avoid other pathological or functional circumstances, such as obesity or diabetes. The model is not replicable in humans as a bariatric technique. This experimental model consists of a pre-duodenal ileal transposition (PDIT). The main goal is to place the ileal portion right after the pylorus. It is then anastomosed to the first portion of the duodenum, this way, the pyloric sphincter keeps its original anatomical disposition even though it is not functional anymore. Our goal is to determine the role of the terminal ileum, when located in an anomalous situation. The change of the anatomical configuration of the digestive tube has been investigated before by different investigation groups but our study provides a new technique, never published before, which brings the transposed ileum as proximal as possible in the digestive tube, right after the stomach to eliminate the foregut bias.
Hence, this way we open up a whole new range of possibilities to study related to the role held by the different portions of the digestive tract such as the terminal ileum, in the improvement of the glycemic metabolism. In this paper, we report a new and feasible model which will lead to new pathways in the specific study of the ileal tract.
Materials and methods
Animals
Every procedure on animals was performed with the approval of the University of Cadiz Committee for the Ethical Use and Care of Experimental Animals. The rats were supplied from the University of Cadiz Animal Production Service, which included the specific laboratories to undergo surgeries. The 30 male Wistar rats were stabled in randomized groups with 15 rats each one of them - an experimental and a surgical control (Sham) group. The specimens were under constant temperature and humidity conditions in a 12-h light/dark cycle, with ad libitum access to normal chow and water. We did not use female rats to avoid the cyclic variations of gonadotropin hormonal effect on the glycemic metabolism. The rats were 12-14 weeks old and weighted around 300-350 g when surgery was undergoing. The survival period was 4 weeks after surgery.
Weight gain and food intake basal glycemia
To evaluate the effect of the surgery in our model, we controlled the weight increase of the animals, as well as the grams of food the animals consumed. The chow intake and the weight increase were quantified every 5 days after surgery for the whole survival period.
Once a week, the basal glycaemia was measured with a glucometer (Glucocard G-Meter 1810, Menarini Diagnostics, Italy) and expressed as mg of glucose/deciliter of blood.
Surgical techniques
The rats were randomly assigned to the experimental group - the PDIT - or to the control group (Sham). Both techniques were performed once the rats were anesthetized with gas (isoflurane). The anesthetic induction was achieved by impregnating a gauze with the same anesthetic after introducing the animal in a close container under an extractor hood to avoid the inhalation of gas by the surgeons. The anesthetic maintenance was obtained by the use of a continuous ventilation pump of isoflurane (between 1 and 3%, depending on the time needed for the procedure, and avoiding cardiorespiratory arrest). It was provided through a mask that included the rat's mouth and snout, and connected to the pump. A heat source underneath the animal was used in longer procedures to avoid hypothermia due to the abdominal cavity exposure. In the end, we tried to reproduce the external conditions similar to the ones in regular surgery and thus, reduce the mortality rate and biases that could interfere in the normal interpretation of the data.
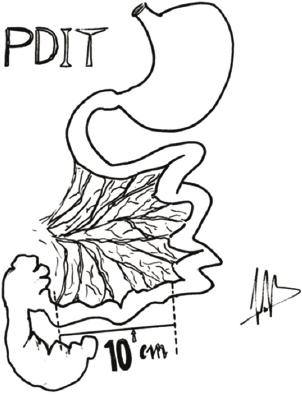
In the PDIT group, the surgical procedure was as followed. The incision made was bisubcostal after cleansing the abdominal wall with chlorhexidine. Then, the whole small bowel was exposed as well as the cecum. Afterward, the stomach was mobilized for a better exposure after liberating the lesser omentum. We measured the past 10 cm of the terminal ileum and divided it (Fig. 1), preserving the vascular supply and the distal edge 1 cm away from the ileocecal valve (Fig. 2). To reduce the mortality in the early samples, the method was modified to reduce the aggression on the ileal vessels. Then, a transverse post-pyloric division was made, closing the duodenal stump with a running suture with polydioxanone (PDS) 5/0. The distal duodenal stump was anastomosed to the distal edge of the transposed ileum with interrupted stitches of PDS 5/0 while the proximal edge of the ileum was anastomosed to the posterior gastric face with continuous suturing with PDS 5/0 after opening the greater omentum (Fig. 3).

Figure 2 This section of ileum and the vessels were located proximally. Duodenum was cutted after pylorum.

Figure 3 Finally, termino-terminal or termino-lateral sutures were made to stablishe the new nutritional flow.
Finally, the last anastomosis made was between the jejunum and terminal ileum, made with interrupted sutures of PDS 5/0. Before closing the abdominal wall, an anesthetic infiltration was performed with 2% mepivacaine diluted in physiological saline solution (1:10). Before closing the abdominal wall with a running suture with Vicryl 2/0, the whole intestinal mass was introduced inside the cavity with warm physiological saline solution (36°C). This surgical technique was always performed by the same main surgeon.
The control group technique (Sham) reproduced the surgical aggression over the digestive tract and the stress of the animal, before and after the surgical procedure but maintained the anatomical disposition of the digestive tube. It was performed by a bisubcostal incision after cleansing the abdominal wall with chlorhexidine allowing the exposure of the small bowel loops. Then, we measured the distance from the angle of Treitz to the ileocecal valve. A transversal enterotomy section was performed at 10 cm of the Treitz angle, without intestinal resection. Then, we made an end-to-end anastomosis with interrupted sutures of PDS 5/0.
The rats from both surgical groups were closely monitored for 2 h after the surgical procedure was completed. Post-operative analgesia was performed by the use of a mixture of 13 ml of ibuprofen (Dalsy) in 500 ml of water. A hyperproteic liquid diet was included 12 h after the surgeries. The diet based on Resource® Protein diluted in water (1:4) was used for 48 h before the introduction of solid standard chow (250g).
Statistical analysis
The measured data were expressed as mean ± standard error of the mean (SEM). Comparisons between both groups were performed using the ANOVA test. Once the non-parametric samples character was established, these data were analyzed with a Mann-Whitney U-test and p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS statistical software, version 24.0.
Results
In this section, the described results report the functional variables measured during the survival period. During this stage, these parameters showed us the adaptive processes to keep a balanced homeostatic glycaemia. Thus, the results of the variables detailed some indirect measurable aspect of the nutrient absorption and posterior pancreatic processing.
Weight gain and chow intake, basal glycemia
The weight evolution, food intake, and basal glycaemia were monitored from post-operative day 1 until the sacrifice, 1 a week. The mean weight per week for each group was expressed in grams. The body weight decreased after procedures in both groups. However, there were no significant differences between any of them at any point (Fig. 4). In both groups, the body weight decreased within the 1st week after surgery and then recovered. In the Sham group, body weight increased slowly and progressively until the end of the study, while the PDIT group presented a weight loss at the 4th week, without recovering the initial weight.

Figure 4 Weight gaining (grams) represented on the Y-axis the experimental (pre-duodenal ileal transposition [PDIT]) and control (SHAM) groups. Time was represented in the X-axis in, 5-days periods. No significant differences were found between PDIT and SHAM group during this period. The surgical PDIT group showed a slight weight loss due to the surgical aggression, but the differences were not significant.
Similarly, the food intake did not show any difference between both groups. The food consumption was reduced in all the employed animals in this study compared to the normal intake measured in the animal laboratory (Science Education Partnership Award).
As well as the average basal glycemia per week, which was expressed in mg/dl, and showed no significant changes were observed in the basal glycemia during the period of the study (Fig. 5). We analyzed the summative interpretation of glycemic - area under the curve - and again, no differences were found.

Figure 5 Basal Glycemia after the fasting period was represented in the Y-axis as glucose mg/dl (mean ± standard error of the mean) in both experimental (pre-duodenal ileal transposition) and SHAM groups along time, represented in weeks in the X-axis. Blood glucose levels did not show significant difference between both groups.
Surgical procedures
Throughout the observation period, six rats out of the 30 rats that we had in the beginning of the study died, which made a 20% of the total mortality rate. In the surgical group, four out of the 15 rats died, which constituted a death rate of 26.6%, while in the Sham group, the mortality rate was the 13% (two out of the 15 rats).
None of the deaths happened, while the surgical procedure was taking place. All deaths occurred after post-operative day 1. All deceased rats died between 24 and 96 h after the surgical intervention. After this, animals were sacrificed after 4 weeks after surgeries. Although the expected weight gown for malnutrition, we did not find any other valuable data.
Discussion
Each day increases the knowledge of bariatric metabolic surgery. This is supported by the daily outbreak of new hypotheses. However, the results of scientific investigations are not conclusive on the mechanism of action of metabolic surgery. In this sense, the ileum is a part of the intestine yet to be studied. Its contributions are very important, but there are many questions to clarify. The previous studies carried out to date are based on an ileal location at the post-duodenal and pre-jejunal level13-16. In addition, generally such ileal interposition was usually associated with another bariatric surgery technique. This article discusses the viability of the transposition of the ileum in a place not described yet (a pre-duodenal localization), without an associated bariatric component. The aim of the study was to know the viability of the model. For this reason, we worked with healthy non-obese rats unlike most of the bibliographic references that are based on studies with diabetic and/or obese animals. Our interest is related to the specific implications of ileum in the resolution of T2DM. Thus, once the model could be well-established, we can follow the cellular participation of ileum at the hormonal level.
The number of complications and mortality was reasonable, although higher than the average mortality obtained in similar previous studies. The overall mortality rate of our study was the 20%, with a mortality lower than the 26% in the surgical group. In addition, none of the deaths occurred during the surgical intervention, always occurred between the first 24 and 96 h postoperatively. Anastomotic leaks and subsequent intraperitoneal infection could be probably the main causes of this mortality rate due to the reintroduction of solid diet and the non-use of antibiotic prophylaxis. Meanwhile, no unusual findings were found during the sacrifice phase. Apart the common peritoneal adhesions, no bowel dilatations or obstruction were observed.
We cannot ignore the possibility of severe metabolic failure due to intense hyperglycemia in the animals, but ketoacidotic symptoms were not observed. Thrombotic or vascular complications, due to the traction over the ileal vessels, might not be excluded. Although we did changes on the initial surgical procedures about the route of ileal vessels. This technical modifications would have helped minimize the mentioned problems. The techniques performed so far in the metabolic surgery field were developed from the bariatric surgery, so weight loss was unavoidable. In our case, we did not find a significant weight loss after the surgery. This supported the results of the previous studies. New studies in a model of diabetic non-obese rats could be done to corroborate these results. The glycemic measurements showed no differences compared to the control group. However, we expected these differences; the rats of the PDIT group could stand a slight lower glycemia, due to a possible improvement in glucose tolerance at the expense of an increase in insulin sensitivity15,16. On the other hand, posterior studies could determine changes in pancreas cellularity that could explain glycemic behavior. This is one of our next analysis of the extracted pancreas.
Regarding the hormonal effect, the Hindgut Theory as well as the Foregut Theory has in common the importance of the role of the digestive tract. Therefore, they are not mutually exclusive. The interposition of the ileum in a post-gastric and pre-duodenal location determined an alteration of the intestinal flow. This conditioned a modification of the incretines and anti-incretines signals. In this respect, it would be interesting to investigate the modifications in the enterohormonal levels (e.g., GLP-1, GIP, PPY, as well as the specific receptors) after this surgical model16,17. The different portions of small bowel will be analyzed to determine the changes in releasing cellularity. Mainly, the GLP-1 releasing L-cells located in the ileum, which has been located in extended location after RYGB18.
Bariatric surgeries, depending on the kind of procedure, had an effect on the concentration of the circulating biliary salts. The terminal ileum, when it was located in an anomalous situation, could determine a change on the circulating levels of the biliary salts. In the ileal lumen, gastric content will be secreted without bile salts and pancreatic enzymes. In addition, the pH will be very acid, straight from the stomach, not buffered yet. This was contributed by a different duodenal situation, distal to the ileum. The lack of enzymes stopped the content and micronutrients from being absorbed. This change could improve the glycemic homeostasis in the diabetic patient19,20.
The modification of the anatomy changed the quality and quantity of absorbed nutrients. The changes must induce in the composition, characteristics, and activity of the intestinal microbiota, which could explain the partial improvement of hydrocarbon metabolism after bariatric surgery. The relationship between the different incretins and the changes in the concentrations of the circulating biliary salts might be important and should be the subject of future studied. Moreover, the nervous system is a whole field to explore, since we preserved the vascularization and the enteral nerves. Therefore, the potential alterations that this technique produced in the normal development of nutrition and metabolism must be considered.
We can conclude that the reported technique is both, new and reasonable, with a relatively assumable mortality rate in an experimental model. More studies are needed in this direction, which could value different animal models and objectivize the real hormonal changes. Our study could open a new range of possibilities in the field of the metabolic surgery, since the improvement of the carbohydrate metabolism in patients after this kind of procedures is still conundrum. The histological analyses are currently being developed. Several studies are in progress: focusing the histology of the pancreas, considering the changes in cellularity of β-cell mass, and the expansions in releasing cellularity of the different portions of intestine. Both kind of studies have been developed in other previous papers6,9,18.
The objective was to obtain an experimental model. The extrapolation of the obtained results to humans is possible. We defend the rational use of this animal model. In this methodological sense, a higher statistical power could have provided stronger and more significant results. Although the objective of the study was well defined, the validity of the surgical model will be better through another series of functional and histological determinations.











 nueva página del texto (beta)
nueva página del texto (beta)