Introduction
Abdominal aortic aneurysm (AAA) describes a segmental, full-thickness dilatation of the abdominal aorta exceeding the normal vessel diameter by 50%, although an aneurysm diameter of 3.0 cm is commonly regarded as the threshold1. The prevalence rates of AAA range from 1.9% to 18.5% in males and 0% to 4.2% in females2. Frequent risk factors associated with AAA are age, smoking, gender, chronic obstructive pulmonary disease, chronic kidney disease, hypertension, family history, and coronary artery disease3. They are usually asymptomatic unless complications occur. Patients at the highest risk of aortic rupture are those with larger diameter AAAs. Growth rates increase markedly with aneurysm diameter; for each 0.5 cm increase in AAA diameter, growth rates increased by 0.5 mm/year and rupture rates double4,5. The estimated annual rupture risk according to diameter is 0%, 0-5%, 13-15%, 10-20%, 20-40%, and 30-50% in cases with diameter less than 4 cm, 4-5 cm, 5-6 cm, 6-7 cm, 7-8, and > 8, respectively6. This catastrophic event is associated with a mortality of 50–80% and even with emergency surgical repair, mortality is about 40% to 50%7,8; the strongest predictor of in-hospital mortality has been found to be age9. There are currently open and endovascular techniques whose objective is to isolate the aneurysm from the circulation, eliminating the risk of rupture. Early complications after the procedure are common. They include endoleaks (persistent blood flow into the aneurysm sac after graft placement), access site complications (arterial rupture and dissection), atheroembolism, lower limbs ischemia, renal failure, and endograft migration.
Recent studies have found a significantly decrease in AAA rupture mortality rates, mainly due to improvements in public health awareness, screening, and management10-12. In view of the high morbidity and mortality rates, the importance of early diagnosis and treatment to decrease the public health burden, this study is aimed to evaluate the characteristics and outcome of patients with AAAs and its correlation with mortality in the first 30 days after the procedure was performed. To the best of our knowledge, this is the first analysis of the characteristics and outcomes of AAA including Mexican population.
Materials and methods
Study design and setting
This is a retrospective, cross-sectional study conducted at a national vascular surgery referral hospital in Mexico. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required. This retrospective study was approved by the institutional ethics review board and a waiver of consent was obtained.
Study population
From January 2016 to December 2021, patients with AAA presenting to the emergency department or in-hospital vascular surgery consultation were studied. For this study, patients with confirmed AAA were enrolled using census sampling method. Patients with an incomplete medical profile and those discharged against medical advice were excluded.
Data collection
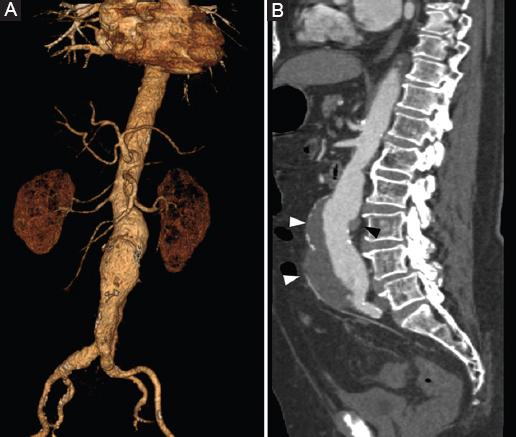
Data were collected by reviewing medical records of the medical center. Pre-designed checklists containing medical history, demographic data (age, gender), chief complaint, characteristics of aneurysm (location, size), family history, presence or absence of leakage based on computed tomography scan findings, and treatment approach, as well as outcomes (mortality) (Fig. 1).
Statistical analysis
Data analysis was done using the Statistical Package for the Social Sciences version 25.0 statistical software. Findings were presented as mean ± standard deviation or frequency (%) for numerical and categorical variables, respectively. The utilized tests were chi-square, independent sample t-test, and Fisher’s exact test. p < 0.05 was considered statistically significant.
Results
Characteristics of patients
During COVID-19 pandemic, the admission of patients reduced significantly, leaving 56 patients for analysis. Table 1 and Figure 2 show the baseline characteristics of studied patients. The mean age was 71.93 ± 10.21 (22-86). 80.4% (45) were male and 19.6% (11) were female. The most frequent chief complaint was pain (51.8%), whereas abdominal pain being the most frequent location (37.5%), followed by lumbar pain (12.5%) and thoracic pain (8.9%). Limb ischemia presented in 7.1% and shock state only in 3.6%. The main duration of pain was 1.65 ± 4.33 months and mean aneurysmal size was 65.42 mm ± 15.26. Location of the aneurysm was found infrarenal in 89.3%, juxtarenal in 5.4%, and abdomino-thoracic aorta in 5.4%. Synchronous aneurysm presented on the right common iliac artery (14.3%), left common iliac artery (3.6%), and both iliac arteries (10.7%).
Table 1 Baseline characteristics of patients
| Variables | Frequency, n (%) |
|---|---|
| Gender | |
| Male | 45 (80.4) |
| Female | 11 (19.6) |
| Pain location | |
| Abdominal | 21 (37.5) |
| Lumbar | 7 (12.5) |
| Thoracic | 5 (8.9) |
| Shock state | 2 (3.6) |
| Limb ischemia | 4 (7.1) |
| Medical history | |
| Smoking | 50 (89.3) |
| Hypertension | 43 (76.8) |
| Ischemic heart disease | 13 (23.2) |
| Diabetes mellitus | 12 (21.4) |
| Chronic kidney disease | 9 (16.1) |
| Dyslipidemia | 6 (10.3) |
| Chronic obstructive pulmonary disease | 5 (8.9) |
| Cerebrovascular accident | 3 (5.4) |
| Iliac artery synchronous aneurysm | |
| Right common iliac artery | 8 (14.3) |
| Bilateral common iliac artery | 6 (10.7) |
| Left common iliac artery | 2 (3.6) |
| Family history | 1 (1.8) |
| Aneurysm location | |
| Infrarenal | 50 (89.3) |
| Juxtarenal | 3 (5.4) |
| Abdomino-thoracic | 3 (5.4) |
Outcomes
Elective procedure was performed in 80.4% (45). Open surgery was performed in 32.1% (18). Of all mortality in open surgery, ruptured aneurysm represented 80% (8). Endovascular procedure was performed in 67.9% (38) with a mortality of 10.5% (4). Ruptured aneurysms represented 19.6% (11) of cases, in which death was seen in 81.8% (9). 25% (14) patients did not survive 30 days after the procedure was performed, in which ruptured aneurysms represented 64.3% (9). Duration of the procedure (p = 0.001), blood loss (p < 0.001), age > 75 years (p = 0.027), aneurysm size > 65 mm (p = 0.01), open surgery (p = 0.001), presence of pain (p = 0.005), chronic kidney disease (p = 0.03), and rupture of the aneurysm (p < 0.001) were among the factors significantly associated with mortality (Table 2).
Table 2 Correlation between baseline characteristics, outcomes, and mortality
| Variables | Survived, n (%) | Died, n (%) | p value | OR (CI 95%) |
|---|---|---|---|---|
| Age > 75 | 13 (59.1) | 9 (40.9) | 0.02 | 4.01 (1.1-14.3) |
| Aneurysm size > 65 mm | 11 (55) | 9 (45) | 0.01 | 5 (1.3-18.4) |
| Open surgery | 8 (44.4) | 10 (55.6) | 0.001 | 10.6 (0.6-42.7) |
| Female gender | 7 (63.6) | 4 (36.4) | 0.43 | 0.5 (0.1-2) |
| Pain | 17 (21.8) | 12 (41.4) | 0.005 | 8.8 (1.7-44) |
| Ruptured aneurysm | 2 (18.2) | 9 (81.8) | < 0.001 | 36 (5.9-216) |
| Cerebrovascular accident | 1 (33.3) | 2 (66.6) | 0.15 | 6.8 (0.5-82) |
| Hypertension | 31 (72.1) | 12 (27.9) | 0.48 | 2.1 (0.4-11) |
| Smoking | 38 (76) | 12 (24) | 0.63 | 0.6 (0.1-3) |
| Diabetes mellitus | 12 (100) | 0 (0) | 0.02 | 0.6 (0.5-0.8) |
| Chronic kidney disease | 4 (44.4) | 5 (55.6) | 0.03 | 5.2 (1.1-23) |
| Ischemic heart disease | 11 (84.6) | 2 (15.4) | 0.48 | 0.4 (0.09-2.4) |
| Chronic obstructive pulmonary disease | 2 (40) | 3 (60) | 0.09 | 5.4 (0.8-36) |
| Length of stay (days) | ||||
| Mean ± DE | 13.1 ± 6.9 | 10.2 ± 10.7 | 0.24 | |
| Duration of procedure (min) | ||||
| Mean ± DE | 233.9 ± 17.2 | 378.5 ± 173.6 | 0.001 | |
| Blood loss (ml) | ||||
| Mean ± DE | 467.6 ± 595 | 2971 ± 2885 | < 0.001 |
Discussion
In this study, we show the characteristics of patients with AAA, the outcomes after the procedure (open or endovascular), and its correlation with mortality in the first 30 days after the procedure was performed (Figs. 3 and 4). According to previous data, smoking is the main risk factor correlated to AAA3. Other risk factors include age, male gender, high blood pressure, coronary artery disease, family history of AAA, high cholesterol, lower extremity peripheral arterial disease, history of a cerebrovascular event, and obesity. Diabetes has been found as a negative association with AAA13. This correlates with our study, in which we observed smoking as the most frequent associated factor, followed by hypertension and coronary artery disease. More recent studies have found a positive correlation between chronic obstructive pulmonary disease, chronic kidney disease, and greater incidence of AAA14,15.
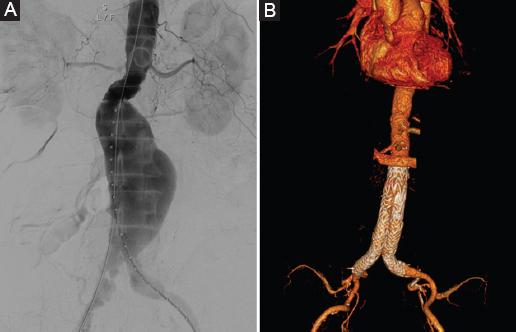
Figure 3 A: diagnostic angiography demonstrating the presence of an infrarenal AAA. B: computed tomography 3D volume rendering after EVAR showing no stent-graft migration, limb occlusion, or endoleak.
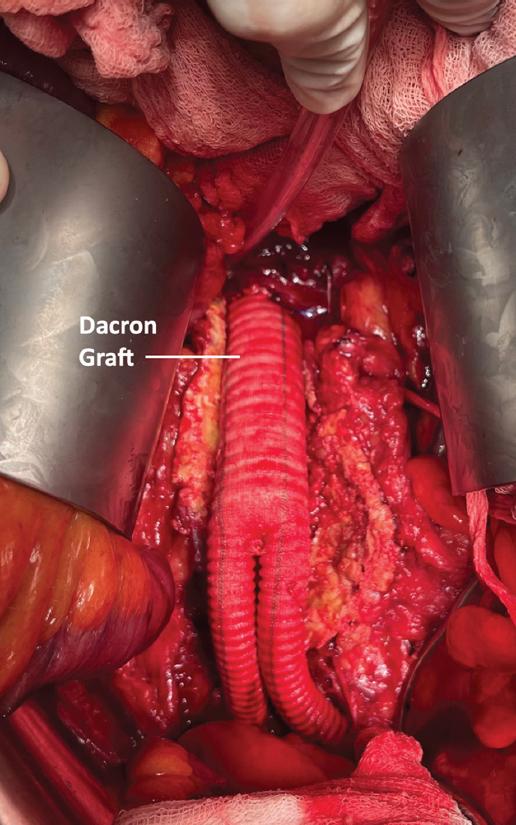
Figure 4 Abdominal aortic aneurism repair with the placement of a dacron graft. Note the aneurysm sac surrounding the graft.
The incidence of concomitant common iliac artery aneurysm has been reported from 12% to 40%, and that right sided is more common than left sided16-18. We report an incidence of 28.6%, also with right sided (14.6%) being more frequent than left (3.6%).
Factors significantly correlated with mortality 30 days after the procedure was performed were the duration of the procedure, blood loss, age > 75 years, aneurysm size > 65 mm, open surgery, presence of pain, chronic kidney disease, and rupture of the aneurysm at presentation. Several predictor models and risk factors for mortality after AAA repair in different clinical situations (elective or urgent; open or endovascular) have been described with contrasting and similar results, but the most consistent data associated with mortality are procedure performed, chronic obstructive pulmonary disease, cerebrovascular disease, renal insufficiency, aneurysm size, increasing age, female sex, serum creatinine level, cardiac disease, previous aortic surgery or stent, abnormal white cell count, and abnormal serum sodium level. Lijftogt et al.19. conducted a systematic review for mortality risk prediction models for AAA surgery and at present, no predictive model is universally applicable due to the lack of external validation, and they also demonstrated highly variable performance across different populations.
Randomized controlled trials20-22 of AAA have shown marked benefits of EVAR with respect to 30-day mortality compared to open repair. Although aneurysm rupture is the most significant complication, aneurysm-related death is a relatively minor determinant of long-term survival in all three randomized trials23, systematic reviews,24 and retrospective studies25,26; atherosclerotic cardiovascular, end-stage renal disease, and cancer-related death represent a greater threat.
Considering that survival is influenced by these factors, this raises the issue of screening for AAA to ease early elective intervention at a younger age, ideally before the onset of comorbidity and therefore, higher risk of death. Evidence shows that screening reduces aneurysm-related mortality in certain populations, with the strongest recommendation for men aged 65-75 years27. Screening patients below 65 years old are unlikely to be economically viable (due to a low prevalence of disease), although expanded criteria for screening have been recently proposed28. It is therefore imperative that aside from perioperative details, patient characteristics and comorbidities are assessed, as well as factors that may affect the outcome to predict the prognosis in patients with AAA. These data might prove to be of clinical interest and relevance for the assessment of prognostic variables for short and long-term survival.
This study has some limitations. First, it is retrospective and therefore prone to inherent bias with such studies. This was a small retrospective study with only 56 patients, and its statistical power may be limited. Second, the follow-up period was lost in some patients as to permit an investigation of the long-term clinical outcomes of overall survival. It is also important to note that several types of graft were utilized; however, this reflects real-world clinical practice.











 nueva página del texto (beta)
nueva página del texto (beta)