Introduction
These are neoplasms made up of spindle cells and/or epithelioid and occasionally pleomorphic cells, which originate from interstitial cells of Cajal (ICC), with mutations in the receptor tyrosine kinase genes, which distinguish them from other tumors.
In the decades from 30 to 50 of the 20th century, these tumors were classified as leiomyomas or leiomyosarcomas and tumors with epithelioid features were designated as leiomyoblastomas or epithelioid leiomyosarcomas.
Dudley cols in 1942 and Rabinovich et al. in 1949 considered that these neoplasms had a benign evolution. In counterpart France and Brenes in 1950, as well as Martin in 1960, they saw that some of these tumors were malignant and also suggest their myoid nature1.
In the decade from 60 to 70, electron microscopy (EM) showed the absence of muscle differentiation. The term gastrointestinal stromal tumor (GIST) was introduced by Mazur and Clark2 in 1983, working with immunohistochemistry (IHC) and ME techniques, determining that they did not have smooth muscle cell characteristics, whereas GIST was occasionally protein positive. S-100 proposes a Schwannian origin from the myenteric plexus.
In 1984, Herrera et al.3 confirmed the neural nature of an intestinal malignancy by calling it plexosarcoma and because it coincided with a publication of a similar tumor with neuroendocrine differentiation by Walker and Dvorak these tumors were classified within the GIST, but considering a possible neuroendocrine differentiation1.
In 1987, Barker and Rudolfe4 succeeded in cloning the c-kit, using somatic human-mouse hybrid cells, locating the gene on chromosome 4. 2 years later, d'Auriol et al.5 located the gene in the 4q11-q12 region.
In 1990, the mesenchymal nature of the tumor was confirmed by IHC, given that between 60% and 70% were positive for CD34 (hematopoiesis progenitor cell antigen), and this is being the first relatively specific marker of the GIST.
Kindblom et al.6 argued that the GIST was related to the ICC, the myenteric plexus, and they form a network located in the plexus of Auerbach, regulating the communication between neurons and muscle fibers, and act as a pacemaker controlling peristalsis, muscle contraction, and possibly as mediators of neurotransmitters7.
Histogenetically, ICC has a mesenchymal origin, and they differ from an intestinal precursor cell which also gives rise to smooth muscle cells. The expression of c-kit proto-oncogene and the precursor cell factor receptor would be necessary for the proliferation and differentiation of the precursor cells toward ICC8.
The absence of neuroendocrine differentiation of ICC, evidenced by EM, excludes that these cells have a bifunctional, neural, and muscular capacity9.
Kitamura et al.10 discovered the increased function by mutation of the c-kit proto-oncogene and overexpression of CD117. Later, Lasota et al.11 demonstrated that c-kit mutations and positivity for c-kit occurred only in GIST. In addition, the interaction between c-kit and its ligand factor precursor cells (stem cell factor) that binds to the intracellular receptor is vital for cell survival, proliferation, and differentiation.
Heinrich et al.12 reported that the possibility of a second receptor involved in the pathogenesis of GIST was raised, especially in those lacking mutations in c-kit, and found a second in the platelet-dependent epidermal growth factor alpha (PDGFRα) receptor.
In 2001, Joensuu et al.13 described the first case of GIST, treated with imatinib, designed for the treatment of chronic myeloid leukemia, but which can act on proteins with tyrosine kinase activity, such as c-kit receptors and PDGFRα receptors.
The aim of this study was to describe the clinical pathological aspects and IHC of the neoplasms diagnosed as GIST, in the Surgical Pathology Unit from Hospital General de México "Dr. Eduardo Liceaga", during the period from July 2010 to May 2017, as well as review the literature relevant to this process.
Materials and methods
We reviewed the cases of mesenchymal tumors of the digestive system, during the period from July 2010 to May 2017, which had lamellae and paraffin blocks, to make additional histological sections if necessary; likewise, they had studies of IHC, for CD117, anti-smooth muscle actin (AAML), and S-100 protein (PS-100).
From the microscopic study and IHC of the mesenchymal tumors, 54 were found which fulfilled the GIST criteria. The microscopic study also allowed obtaining data regarding histological pattern, number of mitosis, histological type, state of the borders, necrosis, and differentiation. From the anatomopathological report, data were obtained on the clinical diagnosis, age and sex of the patient, and size and location of the tumor, and with all this information, an overview of the risk factors was formed, which determine the malignant behavior of these neoplasms.
Results
In 54 cases of GIST, the clinical diagnosis was of tumor in 28 cases (51.9%), of probable GIST in 21 (38.9 %), gastric Ca in 3 cases (5.6%), perforation of 1 case (1.9%), and acute abdomen in 1 case (1.9%). The average age of the group was 54 years, with limits between 22 years the least and 81 years the highest. Regarding sex, 29 cases (53.7%) were women and 25 (46.7%) were men. The ratio of women to men is 1.2:1.
Regarding localization, 26 cases (48.1%) were in the stomach, 5 (9.3%) in the duodenum, 8 (14.8%) in the jejunum, 9 cases (16.7%) in the ileum, 3 (5.6%) in the rectum, 2 (3.7%) in omentum, and 1 (1.9) in the mesentery. When correlating the location with the age group, it was found that, in 24 cases (44.4%), it was between 21 and 50-year-old, 25 cases (46.3.3%) between 51 and 75-year-old, and 5 (9.3 %%) >75-year-old (Table 1). The size of the tumors could only be obtained in 44 of the 54 cases and ranged from 1 cm the least to 30 cm the greatest, with an average of 8 cm. (Fig. 1); nevertheless, tumors of 1 cm only there were 1 (2.3%) and tumors > 10 cm. 13 (29.6%) (Table 2).
Table 1 Age and location
| Age groups | Locations | ||||||
|---|---|---|---|---|---|---|---|
| Stomach | Duodenum | Jejunum | Ilium | Rectum | Epiplon | Mesentery | |
| <20 years | |||||||
| 21-50 years | 10 | 4 | 4 | 5 | 1 | ||
| 51-75 years | 13 | 1 | 4 | 3 | 1 | 2 | |
| >75 years | 3 | 1 | 1 | 1 | |||
| Total | 26 | 5 | 8 | 9 | 3 | 2 | 1 |

Figure 1 Macrophotography of duodenal gastrointestinal stromal tumor, well limited, rounded, grayish brown and fasciculate appearance.
Table 2 Size and staging of neoplasias in 44*
| Cases | ||||
|---|---|---|---|---|
| Location | < 2 cm | 2 cm < 5 cm | > 5 cm < 10 cm | > 10 cm |
| T1 | T2 | T3 | T4 | |
| Stomach | 5 | 7 | 7 | |
| Duodenun | 5 | |||
| Yeyunum | 1 | 1 | 1 | |
| Ilium | 1 | 2 | 3 | 4 |
| Rectum | 1 | 1 | ||
| Epiplón | 2 | 2 | ||
| Mesentery | 1 | |||
| Total | 3 (6.8%) | 14 (31.8%) | 14 (31.8%) | 13 (29.6%) |
*Ten cases were biopsies or cases of revision of lamellae, therefore there is no data on the size of the tumor.
Regarding the mitosis index for 50 high-gain fields (CGA, by its abbreviation in Spanish), we found < 2.32 cases (59.3%); > 2 < 5 mitosis for 50 CGA, 9 (16.7%); > 5 < 10 mitosis for 50 CGA, 6 (11.1%); and > 10 mitosis for 50 CGA, 7 (12.9%) (Table 3).
Table 3 Index of mythosis for 50 fields of great increase
| Location | < 2 to 2 | 2 to < 5 | > 5 to < 10 | > 10 |
|---|---|---|---|---|
| Stomach | 18 | 3 | 2 | 3 |
| Duodenun | 5 | |||
| Yeyunum | 5 | 1 | 1 | 1 |
| Ilium | 3 | 3 | 2 | 1 |
| Rectum | 1 | 1 | 1 | |
| Epiplón | 1 | 1 | ||
| Mesentery | 1 | |||
| Total | 32 (59.3%) | 9 (16.7%) | 6 (11.1%) | 7 (12.9%) |
Regarding the histological type, the fusiform variety (Fig. 2) was present in 44 cases (81.5%), the epithelioid form (Fig. 3) in 4 cases (7.4%), and mixed type (Fig. 4) in 6 cases (11.1%). Regarding the borders, 41 cases (78.8%) had rounded edges and 11 (21.2%) had infiltrating edges. In the cases with infiltrating edges, 6 tumors were gastric, 2 of jejunum, 2 of ileum, and 1 of mesentery. Two more cases corresponded to biopsies, and it was not possible to determine the characteristics of the infiltration.

Figure 2 Microscopic image of gastrointestinal stromal tumor with a fusocellular pattern and a mitosis figure in the central part of the HE ×200 image.
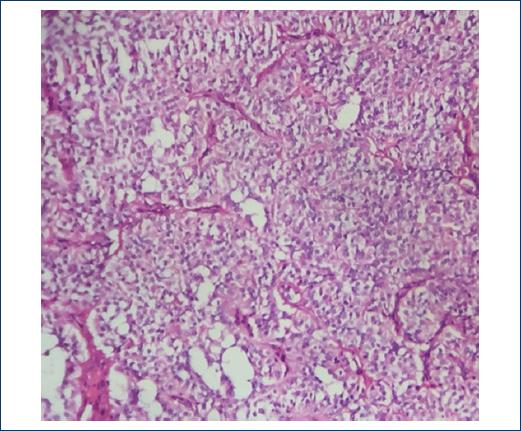
Figure 3 Gastrointestinal stromal tumor of epithelioid type with a pseudoalveolar histological pattern HE ×200.

Figure 4 Microphotography showing a mixed image of gastrointestinal stromal tumor, a fusocellular pattern and an epithelioid HE ×400.
In the IHC study of the 54 cases, all were positive for CD117 (Fig. 5) and the reactions for AAML and PS-100 were negative. In four cases, lymphadenectomy was performed, and in one case of high-grade jejunum GIST, there was metastasis to a regional lymph node (Fig. 6).
Discussion
GIST is neoplasms of mesenchymal origin, constituting a group of lesions characterized immunohistochemically by expressing in >90% of cases the transmembrane receptor derived from the stem cell, with activity on the receptor tyrosine kinase known as CD117 or c-kit.
The incidence of GIST is 10-20 cases per 10,00,000 inhabitants. It occurs around 50 years with an average of 55-65 years. In our cases, the youngest was 22-year-old and the oldest 81-year-old, with an average of 54 years, which agrees with that reported in the literature. It is most commonly located in the stomach (50%-60%), followed by the small intestine (20%), colon and rectum (10%), and esophagus (<5%). Occasionally, they are located in omentum, mesentery, retroperitoneum, pancreas, and gallbladder14. In our tumors, it was in descending order: the stomach (48.1%), small intestine (40.8%), rectum (5.6%), omentum (3.7%), and mesentery (1.9%).
The symptoms depend on the size of the GIST; thus, gastric tumors present with abdominal pain or hemorrhage. In GIST of the small intestine are pain, hemorrhage or signs of obstruction15. In the Mexican population, Medina et al.16 found that the main symptoms are abdominal pain (56%), digestive tract hemorrhage (38.7%) anemia (34.1%), vomiting (16.1%), abdominal distension (12.9%), weight loss (12.9%), and postprandial fullness (6.5%).
The reported size of the tumors is between 0.3 cm the smallest and 38 cm the oldest. We found that the largest tumor was 30 cm and the smaller than 1 cm with an average of 8 cm. As for gender, they occur more frequently in men; however, in our casuistry, the woman was mostly affected in a 1.2:1 ratio.
Within the organ affected by the tumor, it may have an intramural, submucosal, or suberosa location. When cut the surface is of variable color depending on the degree of hemorrhage, its color may be grayish, whitish, reddish, or brownish. They are usually fleshy looking solids, with cystic or necrotic areas17. Of our cases, 13 had necrosis, 10 of which measured >10 cm and 3 <10 cm.
Histologically, GIST presents different cell morphologies: spindle cells (77%), epithelioid cells (8%), and the mixed form (15%)14. The proportion found in our casuistry was spindle cells (81.5%), cell epithelioid (7.4%), and mixed variety (11.1%).
Fusocellular tumors are composed of cells with a fusiform nucleus, scarce eosinophilic or pale cytoplasm, and a fibrillar aspect. They grow without a defined pattern, fusocellular, verticillate, storiform, or palisading, like peripheral nerve tumors. In the cases of this report, we found two with neurofibroma-like pattern, one with a storiform pattern, and the other with cellular pleomorphism.
Epithelioid tumors have extensive, eosinophilic, oncocytic, or clear cytoplasm; they can present perinuclear glycogen, and the histological pattern can be organoid, trabecular, alveolar, or insular. Mixed tumors show transition between the epithelioid and spindle cell fields.
Between 80% and 100% of GISTs show mutations in one or both tyrosine kinase receptors, which are the kit gene and PDGFRα. Tyrosine kinase is detectable by IHC with CD117 antigen, which produces a strong and diffuse staining cytoplasmic. Our cases were all positive (54/54) to CD117.
A small proportion of GIST is negative for CD117; in this situation, a marker that is independent of the kit or PDGFRa mutations has been described, and it is a protein of the calcium and chlorine regulatory channel called DOG 1 (Anoctamin 1). It is an antibody with greater sensitivity to CD117 but with relative specificity, since it has been positive in several carcinomas and some sarcomas18,19. Negative cases of DOG and kit can be diagnosed with the protein kinase theta, which is expressed in all GISTs regardless of their mutational status20.
The mutation of the kit gene is an early event in GIST, with the mutation of exon 11 being the most common. Secondary mutations are also found in exons 13, 14, 17, or 18. Studies of mutations are necessary when GISTs do not react to CD11719,21.
Approximately 10% of GISTs do not detect mutations in c-kit or PDGFRa and it is called wild-type (WT); in spite of not detecting these mutations, the tyrosine kinase is activated. In the GIST of the WT variety, several oncogenic mutations have been described, such as BRAF, which encodes a serine/threonine protein kinase, which plays an important role in the regulation of the cell cycle and oncogenic modification of cellular responses to growth signals via Mitogen-activated protein kinase22.
Between 2005 and 2006, Miettinen and Lasota23 added the location parameter to the Fletcher24 classification, finding that the intestinal GIST of the jejunum and ileum with a similar size and mitosis activity to the gastric ones are more aggressive. In our cases, there are few examples and we do not have data on the evolution after surgery, of the GIST reported here, to reach these conclusions (Tables 2 and 3). However, in Mexico, Medrano et al.25 found, in a study of 66 cases of GIST, that the variable that showed statistical significance in survival was localization, and in intestinal lesions, the survival was lower.
In 2010, the International Union Against Cancer (UICC)26 presented a new classification TNM: T1 tumor <2 cm, T2 tumor >2 cm >5 cm, T3 tumor >5 cm <10 cm, and T4 tumor >10 cm. According to this classification, our cases behaved as follows: T1, 3 cases (6.8%); T2, 14 cases (31.8%); T3, 14 cases (31.8%); and T4, 13 cases (29.6%) (Table 2).
The same UICC ensures the histological grade according to the number of mitoses by 50 CGA: low grade, when the mitosis count is <5 per 50 CGA, and high grade, when the count is >5mitosis per 50 CGA. Regarding the histological grade, our cases presented the following behavior: low grade 41 cases (75.9%) and high grade 13 cases (24.1%) (Table 3).
The prognostic factors to be considered in the GIST are several and include localization, and tumors that originate in the small intestine and rectum have a worse prognosis24. Peritoneal or hepatic metastases are of worse prognosis.
Small tumors, incidental in the serosa, have a favorable course27. Other factors are tumor size, number of mitoses per 50 CGA, spontaneous or iatrogenic rupture of the tumor, affected surgical margins, necrosis, nuclear atypia, muscle, or mucosal invasion28. Ki 67 >10% is associated with poor prognosis31. In the Mexican population, Martínez et al.29 found that the expression of p53 is greater in lesions of the intestine than in the stomach. Ki 67 >10% is associated with poor prognosis30.
The treatment of choice is complete surgical resection; lymphadenectomy is not necessary since lymphatic dissemination is unlikely31. Lymphadenectomy was performed in 4 of our cases, and one of them identified metastases in 1 lymph node.
GIST is resistant to radio- and chemo-therapy and has recurrence or metastasis in 20%-50% of patients with resectable tumors; nevertheless, imatinib, in the postoperative period, has managed to improve recurrence-free survival. With imatinib, the best results are given when there is a mutation of exon 11 and greater resistance with mutations of exon 9 and the PDGFRa gene. When there is resistance, second-generation chemotherapy drugs such as sunitinib or regorafenib can be used32.
The application of micro-RNA (myRNA) in the treatment of GIST is under the study, and they are agents that can provoke an immune response17. The miRNA, which is small single-stranded RNA encoding 19-22 nucleotides, has the ability to regulate gene expression by translational inhibition or degradation of messenger RNA33.
Early diagnosis and radical resection of the primary lesion are the most appropriate treatment for healing.
In our cases, the main treatment used was surgical resection, and we do not have data on the subsequent evolution of patients.











 nueva página del texto (beta)
nueva página del texto (beta)




