Introduction
Limbal stem cell deficiency is a disabling condition, with notable personal, social and economic consequences. It occurs frequently in the consultation and constitutes a therapeutic challenge. Causes of limbic insufficiency can be divided into hereditary and acquired. Among the former are aniridia, congenital epidermal dysplasia, dyskeratosis congenita, Turner syndrome and keratitis associated with multiple endocrine deficiency; among acquired ones are chemical (alkali or acid) or thermal burns, chronic inflammation and scarring processes such as mucous membrane pemphigoid, Stevens-Johnson syndrome, graft-versus-host disease, and chronic limbitis; iatrogenic injuries from radiation, cryotherapy, or topical chemotherapy, contact lens wear, as well as secondary to other ocular surface injuries such as extensive microbial keratitis, neurotrophic keratopathy (neural and ischemic), bullous keratopathy, and extensive surface tumors eyepiece1,2.
The sequelae of limbic insufficiency are complex to manage and can be disabling. Corneal opacities are considered the fifth most frequent cause of blindness around the world, accounting for 5.1% of all cases3. Over the years, various treatments have been proposed, however the only one that has been effective in rejuvenating the corneal surface and restoring vision has been the graft of stem cells from healthy limbic tissue, particularly from the other eye, when possible., or in bilateral cases, from related or cadaveric living donors4-8. The choice of one technique or another will depend on various factors such as the degree of ocular damage (partial or total, unilateral or bilateral), the availability of laboratory resources, and the experience of the surgeon9. Since Dr. Barraquer first introduced his corneal-limbus-conjunctival epithelium transplantation technique in 1965, various researchers began to develop various surgical strategies. For example, Thoh successfully performed a conjunctival transplant in 1977 as a treatment for eye burns. Kenyon10 and Tseng11 improved this technique by incorporating limbal cell transplantation, proposing the conjunctive-limbar autograft (CLAU) in 1989. Later, Pellegrini and collaborators in 1997 proposed the ex-vivo culture transplantation of limbal epithelial cells (CLET) as an alternative. for both unilateral and bilateral lesions with satisfactory results.
CLAU is a simple technique that is performed in a single surgical act, but in which it is required to obtain a large amount of tissue from the eye contralateral to the lesion, as well as skill on the part of the surgeon to obtain this 10-11. CLET, on the other hand, uses less tissue from the contralateral eye, but has the disadvantage that a specialized laboratory is required for tissue growth (cell culture) and consequently the expense is higher. Both techniques have shown good long-term results, however, it is not always possible to perform an autologous transplant, requiring the use of living related or cadaveric donors through allogeneic keratolimbar tissue transplantation (KLAL)12.
More recently, Dr. Virender Sangwan13 and his team combine the positive factors of both techniques (CLAU and CLET), reducing their negative aspects, this is now known as simple limbal epithelial cell transplantation (Simple Limbal Epithelial Transplantation-SLET)14 Originally, this technique consists of the transplantation of limbal stem cells from the contralateral healthy eye to the diseased eye, using a 2x2 mm tissue, cut into small fragments and fixed with tissue adhesive on an amniotic membrane, which serves as a substrate to stimulate the tissue proliferation; however, over time the technique has been adapted and modified with the use of allogeneic tissue for bilateral cases15,16. Since then, many cases have been published with extremely favorable results and minimal complications17-19.
Following the premise that SLET improves visual acuity up to two lines of vision and improves ocular surface conditions by measuring symbepharon, neovascularization, opacity, corneal conjunctivalization and keratinization20, the limbal cell graft from a cadaveric donor (allogeneic), without ex vivo culture, reported in the literature as a therapeutic option for patients with bilateral limbic insufficiency, could substantially improve visual acuity and ocular surface conditions. The main objective of this study is to evaluate the clinical results of limbal cell graft in patients with bilateral limbic insufficiency.
Materials and Methods
A prospective, longitudinal and observational pilot study was carried out at the Hospital General de México “Dr. Eduardo Liceaga” in the department of cornea and refractive surgery. There was a 6-month follow-up to the patients in this study, the first serie report in our hospital. Patients of indistinct gender and age were included, with diagnosis of bilateral limbic insufficiency without active inflammation, without determining aetiology in particular; patients wished to participate and were kept under close follow-up by attending their scheduled appointments.
Classification of bilateral limbal stem cell deficiency
The diagnosis of limbic insufficiency syndrome was made by a single physician in all cases, it was classified into the different stages according to the Sotozono et al.20 system (Table 1). A complete ophthalmologic examination was performed with a slit lamp and fluorescein staining. Evaluation of the posterior segment was performed by ultrasound.
Table 1 Stages of limbic insufficiency by clinical characteristics
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | |
|---|---|---|---|---|
| Conjunctivalization | Absent | < 1/4 corneal surface | 1/4 mid-corneal surface | > half corneal surface |
| Neovascularization | Absent | Confined to peripheral cornea | Extension to pupil margin | Extension beyond the pupil margin to the central zone |
| Opacity | Clear cornea with visualized iris and details | Partial opacity, partial loss of iris detail | Iris details not visualized with barely visible pupil margin | Total opacity, iris and pupil not perceptible |
| Keratinization | Absent | < 1/4 corneal surface | 1/4 mid-corneal surface | > half corneal surface |
| Symblepharon | Absent | Conjunctival involvement | Extension to limbo | Extension to central cornea |
Success and failure of cadaveric donor limbal stem cell graft
The success of the transplant was assessed based on 6 objective criteria: visual acuity, symbepharon, conjunctivalisation, vascularisation, keratinisation and corneal opacity. Success was determined if improvement was found in at least 4 of the 6 criteria; additionally, failure was determined if at least 1 of the following parameters occurred: persistent epithelial defect, central 8 mm conjunctivalization, microbial keratitis, need for retransplantation due to rejection or loss of limbic tissue.
Obtaining limbal stem cell tissue
Limbic tissue was obtained from cadaveric donor sclerocorneal caps, remnants of penetrating keratoplasty surgeries carried out at the General Hospital of Mexico in accordance with the guidelines established by the National Transplant Center (CENATRA). Said tissue was stored in Optisol-GS (Bausch & Lomb) as a preservation medium for an approximate time of 7 to 10 days, refrigerated at 4°C in the eye bank of our hospital; and transported to the operating room the day of surgery. The relatives of the cadaveric donor were informed of its use for this study prior to taking the sclerocorneal cap and a written informed consent was requested.
Surgical procedure
Limbic tissue from a cadaveric donor, radio-sterilized amniotic membrane with Co-60 and tissue adhesive were used as material for surgery. The surgeries were performed by a single surgeon. Fibrovascular tissue was excised from the ocular surface with 360º peritomy and corneal polishing, amniotic membrane was placed on the ocular surface, fixed with tissue adhesive and subsequently the limbic tissue fragments were placed on the membrane in a clockwise direction, leaving the visual axis free.
Results
Six patients with bilateral limbal stem cell deficiency and one with unilateral deficiency who rejected the option of graft of limbal cells from the contralateral eye were included for study. Of these patients, six (85.7%) were male and one (14.3%) female. The mean age was 34.1 years (range 16-59 years), median 25 ± 19.9 years. The most common etiology was corneal burn, observed in four patients with a percentage of 57.14%, it is observed more frequently in males of productive age, due to the type of work activities, in second place three patientes presented Stevens Johnson Syndrome, percentage of 42.86%.
The extent of limbic cell deficiency was total (12 meridian involvement) in six (85.7%) patients and partial (<6 meridian involvement) in one (14.3%) patient. The time of evolution of the underlying pathology is distributed as follows: four patients was 10 years, two patients with more than 10 years and only one patient with an evolution of less than 1 year. Of the total number of patients, fve patients have a history of surgical management with an amniotic membrane graft in the acute process. Table 2 summarizes demographic characteristics of the cohort.
Table 2 Demographic characteristics of the study population
| Characteristics | No. | % |
|---|---|---|
| Gender | ||
| Male | 6 | 85.71 |
| Female | 1 | 14.29 |
| Lateralidad | ||
| Right | 3 | 42.86 |
| Left | 4 | 57.14 |
| Etiology | ||
| Burns | 4 | 57.14 |
| SSJ | 3 | 42.86 |
| Evolution time (years) | ||
| < 1 | 1 | 14.29 |
| 1 - 5 | 2 | 28.57 |
| 5 - 10 | 2 | 28.57 |
| Ø 10 | 2 | 28.57 |
| Extension of limbar insufficiency | ||
| Total (12 h) | 6 | 85.71 |
| 6-11 h | 0 | 0 |
| Partial (<6 h) | 1 | 14.29 |
| Previous surgeries | ||
| IMA | 5 | 71.43 |
| Complications | ||
| Persistent epithelial defec | 1 | 14.29 |
| Graft loss | 1 | 14.29 |
| Membrane detachment | 2 | 28.57 |
| Corneal perforation | 1 | 14.29 |
* SSJ: Steven Johnson syndrome.
** IMA: amniotic membrane graft.
The baseline visual acuity parameters (BVS) were: three patients with finger counts representing 42.85% (3/7), two patients with hand movements representing 28.57% (2/7), one patient with 20/200 and one with 20/60 representing 14.29% respectively (1/7). The baseline clinical characteristics are listed below in Table 3, prior to limbal cell grafting.
Table 3 Baseline characteristics before limbal cell transplantation from a cadaveric donor
| Basal characteristics | No. | % |
|---|---|---|
| Visual acuity | ||
| Perceive light | 0 | 0 |
| Hand movement | 2 | 28.57 |
| Counting fingers | 3 | 42.86 |
| 20/200 | 1 | 14.29 |
| 20/60 | 1 | 14.29 |
| Symblepharon | ||
| G 0 | 0 | 0 |
| G 1 | 3 | 42.86 |
| G 2 | 2 | 28.57 |
| G 3 | 2 | 28.57 |
| Neovascularization | ||
| G 0 | 0 | 0 |
| G 1 | 1 | 14.29 |
| G 2 | 2 | 28.57 |
| G 3 | 4 | 57.14 |
| Opacity | ||
| G 0 | 0 | 0 |
| G 1 | 1 | 14.29 |
| G 2 | 4 | 57.14 |
| G 3 | 2 | 28.57 |
| Conjunctivalization | ||
| G 0 | 0 | 0 |
| G 1 | 0 | 0 |
| G 2 | 4 | 57.14 |
| G 3 | 3 | 42.86 |
| Keratinization | ||
| G 0 | 0 | 0 |
| G 1 | 2 | 28.57 |
| G 2 | 3 | 42.86 |
| G 3 | 2 | 28.57 |
G0: grade 0; G1: grade 1; G2: grade 2; G3: grade 3.
Evaluation of the limbal stem cell graft from cadaveric donor
At the final follow-up visit after the graft at 6 months, the seven patients maintained a stable corneal surface and with clinical improvement of symblepharon, neovascularization, conjunctivalization, opacity and keratinization (Fig. 1). Only two patients (28.57%; 2/7) presented a persistent epithelial defect in the first months of follow-up, which improves with the use of 50% platelet-rich plasma and lubricants. Only one patient (14.29%; 1/7) presented partial graft loss <50% of the implanted tissue with response to residual tissue and without requiring retransplantation. None of the patients presented central 8 mm conjunctivalization, microbial keratitis, or rejection.
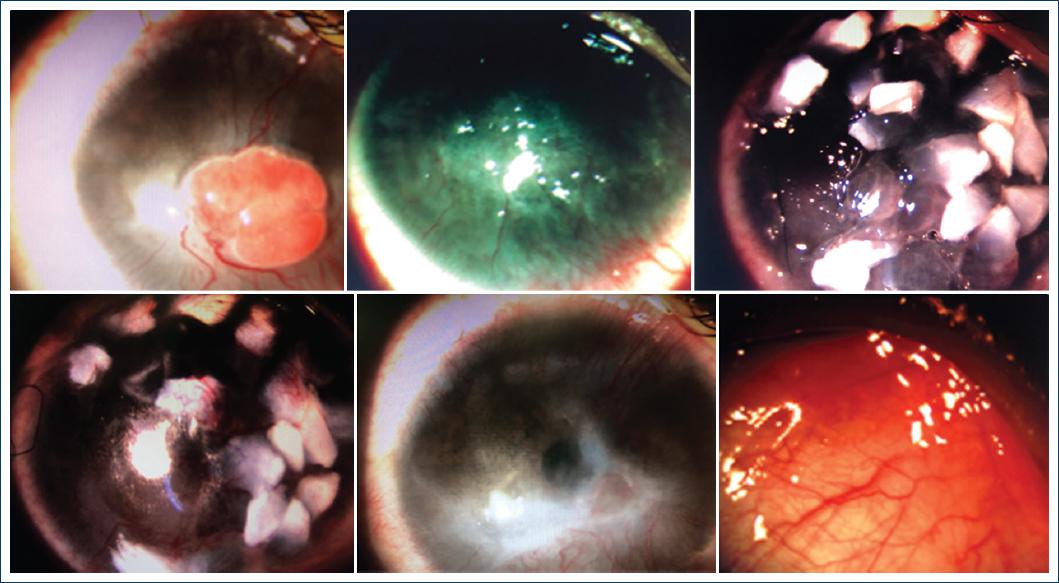
Figure 1 Photographs of the clinical evolution of a 17-year-old male patient with bilateral alkali corneal burn, development of pyogenic granuloma in the right eye. 1st. Pyogenic granuloma 2 months after corneal burn. Post-surgical photograph of resection of a pyogenic granuloma, showing limbal cell deficiency greater than 180º, deep neovascularization, central dense opacity, visual acuity of Finger Count. 1 week after a cadaveric donor allogeneic limbal cell transplantation. 1d. 1 month after allogenic SLET. Same eye 3 months after cadaveric allogeneic SLET, shows 360º peripheral neovascularization, conjunctivalization, re-epithelialization and transparency in visual axis, visual acuity 20/150. Right eye diminished symblepharons.
The objective clinical criteria to determine the success of the transplantation were visual acuity, degree of symblepharon, conjunctivalization, vascularization and corneal opacity, comparing the baseline stage, at 3 months and 6 months of follow-up.
Visual acuity (VA) was classified on a numerical scale from 0 to 5, being 0: 20/60; 1: 20/150; 2: 20/200; 3: finger counting (CD), 4: hand movement (MM); 5: perceives light (PL). The AVB with an average of 3.43 (CD) and average range 2.29 (20/200). AV6 with a mean of 2.71 and an average range of 1.93 (20/150). No significant difference (p = 0.504) was observed in VA both from baseline (BVS) and at 6-month follow-up.
The symblepharon was classified by grades ranging from 0 to 3, the results of the baseline and 6 months of follow-up are listed below: baseline symblepharon, three patients were reported in grade 1 (3/7), two patients in grade 2 (2/7) and two patients in grade 3 (2/7) with a mean of 1.86 and a mean range of 2.86; With a 6-month follow-up, three patients were reported in grade 0 (3/7), three patients in grade 1 (3/7) and one patient in grade 2 (1/7) with a mean of 0.71 and a mean range of 1.50. A significant difference (p = 0.007) in symbology was observed from baseline to 6 months of follow-up.
Neovascularization was classified by grades ranging from 0 to 3, the results of the baseline and 6 months of follow-up are listed below: baseline neovascularization, four patients were reported in grade 3 (4/7), two patients in grade 2 (2/7) and one patient in grade 1 (1/7) with a mean of 2.43 and a mean range of 2.71; Neovascularization 6 months of follow-up, three patients were reported in grade 2 (3/7), three patients in grade 1 (3/7) and one patient in grade 0 (1/7) with a mean of 1.29 and a mean range of 1.57. A significant difference (p = 0.009) in neovascularization was observed from baseline to 6 months of follow-up.
The opacity was classified by degrees ranging from 0 to 3, the results of the baseline and 6 months of follow-up are listed below: baseline opacity, four patients were reported in grade 2 (4/7), two patients in grade 3 (2/7) and one patient in grade 1 (1/7) with a mean of 2.14 and a mean range of 2.71; opacity 6 months of follow-up, five patients were reported in grade 1 (5/7), onepatient in grade 2 (1/7) and one patient in grade 3 (1/7) with a mean of 1.43 and a mean range of 1.79. A significant difference (p = 0.016) in opacity was observed from baseline to 6 months of follow-up.
Conjunctivalization was classified by grades ranging from 0 to 3, the results of baseline and 6 months of follow-up are listed below: baseline conjunctivalization, four patients were reported in grade 2 (4/7) and three patients in grade 3 (3/7) with a mean of 2.43 and an average range of 2.93; Conjunctivalization 6 months of follow-up, three patients were reported in grade 2 (3/7), three patients in grade 0 (3/7) and one patient in grade 1 (1/7) with a mean of 1.00 and a mean range of 1.64. A significant difference (p = 0.004) in conjunctivalization was observed from baseline to 6 months of follow-up.
Keratinization was classified by grades ranging from 0 to 3, the results of the baseline and 6 months of follow-up are listed below: baseline keratinization, three patients were reported in grade 2 (3/7), two patients in grade 1 (2/7) and two patients in grade 3 (2/7) with a mean of 2.00 and a mean range of 3.00; keratinization 6 months of follow-up, five patients were reported in grade 0 (5/7), one patient in grade 1 (1/7) and one patient in grade 2 (1/7) with a mean of 0.29 and average range of 1.43. A significant difference (p = 0.001) in keratinization was observed from baseline to 6 months of follow-up.
Finally, when comparing the baseline clinical criteria, at 3 months and 6 months of follow-up, it is found that the VA did not have a significant difference (p = 0.504) or the opacity found in the study subjects in this follow-up period (p = 0.016), however, there is a significant difference in the other criteria such as symblepharon (p = 0.007), neovascularization (p = 0.009), conjunctivalization (p = 0.004) and keratinization (p = 0.001). Table 4 summarizes the results of each clinical criterion from baseline, 3 months, and 6 months. As in Figure 2, the results are visually summarized in the established time periods.
Table 4 Results in the established periods
| Results | Basal | 3 months | 6 months | Square chi |
|---|---|---|---|---|
| Visual acuity (VA) | 2.29 | 1.79 | 1.93 | p = 0.504 |
| Opacity | 2.71 | 1.50 | 1.79 | p = 0.016 |
| Symblepharon | 2.86 | 1.64 | 1.50 | p = 0.007 |
| Neovascularization | 2.71 | 1.71 | 1.57 | p = 0.009 |
| Conjunctivalization | 2.93 | 1.43 | 1.64 | p = 0.004 |
| Keratinization | 3.0 | 1.57 | 1.43 | p = 0.001 |
Discussion
The success of the limbal cell graft from a cadaveric donor is confirmed by having improvement in 4 out of 6 clinical criteria; In our study, 5 clinical criteria were observed with a statistically significant difference from baseline measurements to 6 months, a satisfactory result.
It was identified that there was no significant difference in visual acuity in our 6-month follow-up, however, two of our patients presented an improvement of more than 2 lines of vision. The ocular surface conditions (symblepharon, opacity, keratinization, conjunctivalization and neovascularization) showed a statistically significant difference, similar to that reported by Campbell et al. who recently studied 30 patients for 32 months with cell culture where the improvement in visual acuity was not significant but the majority of patients in both groups ended up with an improved score at 18 months; in contrast to ocular surface conditions with initial nonsustained significant improvement returning to baseline levels around 18 months of follow-up.
SLET is the most promising current technique, with good reported results and success ranging from 60-75%21,22, however, it requires a minimum of donor tissue from the healthy eye, being impossible to perform in patients with bilateral limbic insufficiency23-26. Compared to SLET, the limbal cell graft from a cadaveric donor in our study proved to have good results, being a therapeutic option for these cases.
Regarding the safety of the cadaveric donor graft, Campbell et al.27 developed a multicenter randomized controlled study in 13 patients with bilateral deficiency to assess the viability, safety and efficacy of allogeneic stem cell grafting. The authors performed DNA analysis of both donor and recipient after allogeneic limbal cell graft and DNA from both was found in the first months; but after 6 months, only receptor DNA was found, which suggests that the graft is transitory, thus justifying that the benefits on the ocular surface are due to the first effects of the stem cells, which could induce the repair of the limbal niche. or stimulating a small number of latent host stem cells to potentially multiply through a paracrine or chemotactic mechanism, however this remains speculative and requires further research. Topical and systemic immunosuppression should be used at least in this window of time to avoid rejection and have long-term benefits on the ocular surface, which is why in this study it was necessary to apply topical immunomodulators for a minimum of 6 months and topical steroids in reduced dose.
The limitations of this report were: the reduced number of patients studied due to the limited economic conditions of the patients and the decrease in volume in organ and tissue donation programs this year. With the results found, it is justified to deepen and expand the sample size and continue with the evaluation of patients who receive this type of management for a longer period of time.
Conclusions
This is a pilot study that analyzes the results in a short term of 6 months of the limbal cell graft from a cadaveric donor, in which it can be determined that it is a successful and reliable technique to improve the conditions of the ocular surface in bilateral limbic insufficiency. but apparently not in visual acuity.
In addition to being an option available for patients without the possibility of limbic cell graft of the contralateral eye that offers improvement of the ocular surface and also a therapeutic option for patients with unilateral disease while maintaining the integrity of the contralateral eye.
This study should be expanded by taking a larger sample of patients and with surveillance for at least one year to obtain more convincing results.











 nueva página del texto (beta)
nueva página del texto (beta)



