Introduction
Isolated iliac artery aneurysms comprise less than 2% of abdominal aneurysms and affect 0.3-0-6% of the general population. The internal iliac artery is affected in 10 to 30% of cases and the aneurysm is bilateral in half of the cases. Iliac aneurysms are associated with abdominal aortic aneurysm in 20% to 30% of cases.
Etiologic factors include trauma, vasculitis, pregnancy, infections, connective tissue disease, and iatrogenesis. Most of the AAIC are asymptomatic and the diagnosis is difficult. They can manifest with pulsating masses, abdominal or lower back pain (acute, caused by expansion or rupture, or chronic due to compression of nerves and organs), urinary symptoms (54%), gastrointestinal symptoms (constipation, tenesmus, pain on rectal examination and bleeding intestinal) and neurological symptoms and thromboembolism caused by compression of the femoral iliac venous system. In most cases patients are asymptomatic unless a rupture occurs. It can be diagnosed by Doppler ultrasound, magnetic resonance or, preferably, angiotomography. Diameters greater than 3 cm and symptomatic cases are an indication for surgery1.
Methods
A review of the number of patients with abdominal aortic aneurysm was carried out with the intention of searching only for iliac artery aneurysms, between January 1, 2018 and April 30, 2022. According to the literature, the most important factors involved in the management of these patients were analyzed.
Results
From the 3 patients with iliac artery aneurysm, two were male and one female, mean age 60 years, average smoking age 15 years in 66%, one patient with diabetes mellitus, two patients with a history of previous abdominal surgery, 70 % corresponded to aneurysm of the common iliac artery, average maximum diameter of the aneurysms 50 mm. One patient was managed with open surgery and two Endovascular. For open surgery, an 8 mm linear ringed PTFE (polytetrafluoroethylene) graft was used, and for endovascular surgery, a total of 5 covered stents. One of the patients with a stent presented an artery rupture and required a blood transfusion. The three patients evolved with total closure of the aneurysm. The 2 endovascular patients were discharged after 48 hours and the open surgery patient remained 96 hours post-surgery. Only one patient required hypogastric embolization. Follow-up in the outpatient clinic was uneventful, with good distal pulses and no ischemic complications Table 1.
Case 1
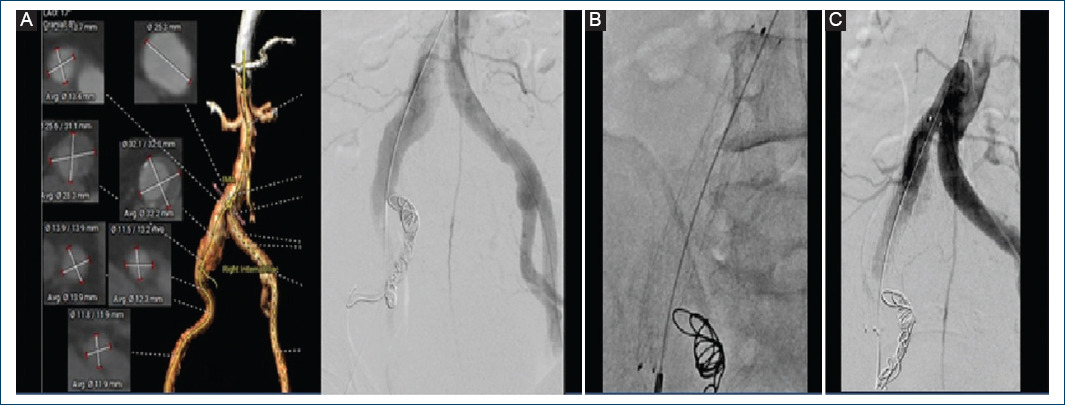
The patient was a 72-year-old female, with a history of schizophrenia of 15 years of diagnosis, under treatment with trifluoperazine and clonazepam, currently controlled, COPD without treatment or follow-up. Surgical history: hysterectomy 10 years ago secondary to uterine myxomatosis. Drug addiction: chronic smoking at a rate of 20 cigarettes/day for 50 years, the rest denied. Current condition: started 2 days ago with pain in the left iliac fossa that progressively radiates to the hypogastrium and right iliac fossa, decreasing the pain spontaneously, abdominal ultrasound reports the presence of a common iliac artery left aneurysm. At physical examination the patient presented soft abdomen, painful on deep palpation in the mesogastrium and left iliac fossa, accompanied by pulsatility. No palpable masses or signs of peritoneal irritation. Lower extremities with arterial integrity pulses 2/2 of good intensity bilateral ITB 1 (Fig. 1).
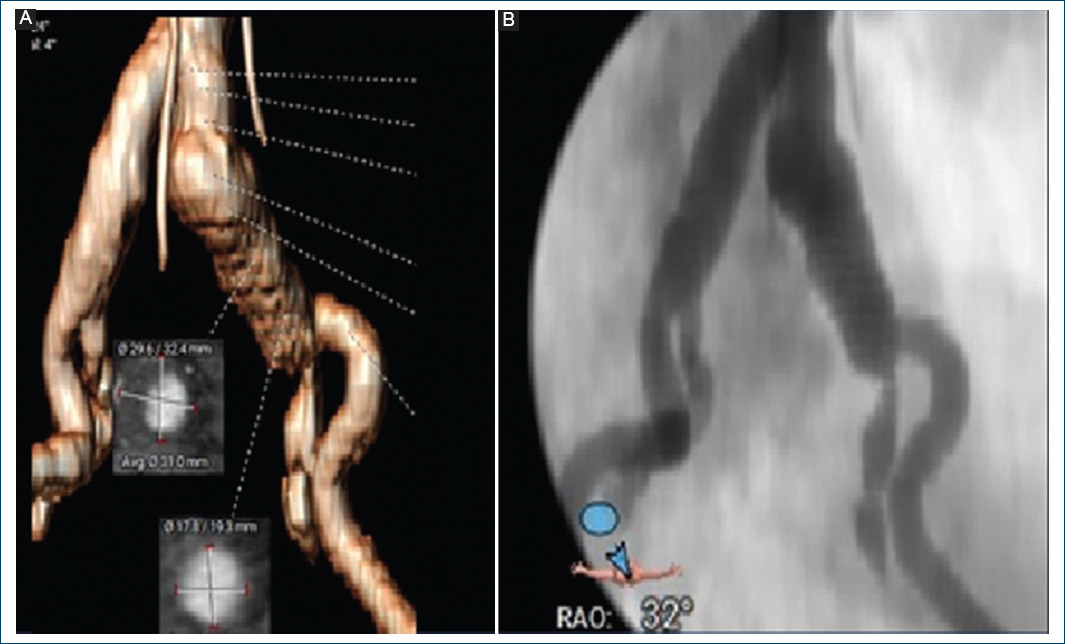
Figure 1 A: 3D CT angiography and arteriography showing left common iliac artery aneurysm. B: neck of 13 mm, largest diameter of the aneurysm of 36 mm and distal neck of 10.6 mm.
3D CT angiography with reconstruction showed the presence of a left common iliac aneurysm with a neck length from the level of the aortic bifurcation of 10 mm in diameter and a diameter of the iliac artery of 13 mm at the proximal level, diameter maximum of the aneurysm is 36 mm with a length of 80 mm ending in the bifurcation of the external and internal iliac artery without dilatation of the hypogastric artery, external iliac distal neck of 10 mm. She is taken to diagnostic and therapeutic arteriography, a 5 Fr right femoral introducer is placed, a 0.35 guide is introduced, a pigtail catheter up to the bifurcation, control arteriography is performed with an injector where the diameters are confirmed. It was decided to perform endovascular treatment with a covered stent, oversize it up to 16 mm. In order to insert the stents, an 18-fr introducer is required, so a dissection of the left femoral artery is performed with proximal and distal vascular control. A 0.35 guidewire is inserted with a centimeter catheter where previous measurements are confirmed, the guide is removed and an amplatzer support is placed through which 3 covered stents are introduced, dispensed by a 16 mm x 38 mm balloon (they only have a measurement of 38 mm in length per 3 stents are required to cover the 80mm length) at the end, control arteriography is performed, vessel rupture is observed with contrast medium leaking into the retroperitoneal area of the distal iliac stent with narrowing in the stent cone at 10 mm, so it is necessary to place a last one of 10 mm x 50 mm coated, arteriographic control shows absence of leakage adequate passage of the contrast medium. Presenting discharge at the time of rupture and through the introducer without repercussions on vital signs, a globular package was given. The patient evolved satisfactorily with good intensity pulses without complications, so she was discharged after 48 hours without complications (Fig. 2).
Case 2
The patient was a 64-year-old male, with a history of type 2 diabetes mellitus of 4 years of evolution on treatment with metformin 500 mg, one tablet orally every 24 hours. Surgical: open cholecystectomy 30 years ago. Tonsillectomy 20 years ago. Left renal extracorporeal lithotripsy 15 years ago, open nephrolithotomy 5 years ago. Drug addiction: smoking from the age of 15 to the present, 15 cigarettes per day. Current condition: started on April 20 with diffuse onset lumbar pain in the left region that did not improve with analgesics. He went to a private urologist due to a history of lithiasis who indicated control laboratories where urinary tract infection was reported. Management with antibiotics was started without improvement. The treating physician performs a simple and contrasted tomography where he reports an aneurysm of the right common iliac artery, he is sent to the emergency room of this hospital. Physical examination shows soft abdomen, not painful on superficial or deep palpation, with no evidence of peritoneal irritation, normal peristalsis, without signs of peritoneal irritation and lower extremities with arterial integrity pulses 2/2 of good intensity bilateral ITB 1 (Fig. 3).

Figure 3 Right compunction iliac aneurysm (RIA) with a 13-mm neck, maximum aneurysm diameter of 32 mm, and a 12-mm distal neck without hypogastric involvement. A: transverse plane. B: sagittal plane. C: coronal plane.
Angiotomography with 3D reconstruction confirms the presence of a right common iliac aneurysm with neck length from the level of the aortic bifurcation of 11 mm in diameter and a diameter of the iliac artery of 13.4 mm at the proximal level, maximum diameter of the aneurysm is of 32 mm with a length of 65 mm that ends in the bifurcation of the external and internal iliac artery without dilation of the hypogastric artery, external iliac distal neck of 12 mm. He is taken to diagnostic and therapeutic arteriography, a 6 fr left femoral introducer is placed, a 0.35 guide is inserted, a pigtail catheter up to the bifurcation, control arteriography is performed where the previous measurements are confirmed. A cross over was performed towards the right iliac femoral artery, a new control arteriography in which we observed an 11-mm hypogastric artery, for which embolization was decided, a guidewire and diagnostic catheter were inserted up to the right hypogastric, once a guidewire and catheter were in the right hypogastric, the catheter was withdrawn and 10 x 25 mm, 12 x 20 mm, 15 x 25 mm coils are introduced with a latency of 5 min. With arteriography, the absence of contrast medium towards the hypogastric region is verified. We proceed to infiltrate 10 ml of anesthesia in the right inguinal region, an incision is made to approach the right common femoral artery, distal and proximal vascular control with longitudinal arteriotomy, placement of a 10-f introducer guided by fluoroscopy up to the common iliac artery, guide 035 is placed; 1 stent is inserted coated dispensed by 13 mm x 96 mm balloon which covers the total length of the aneurysmal lesion, control arteriography was performed without the presence of endoleak and toral closure of the sac. Atheriotomy was closed with 6-zero vascular prolene and closure by planes. The patient evolved satisfactorily with good intensity pulses without complications, so he was discharged after 48 hours without complications (Fig. 4).
Case 3
The patient was a 45-year-old male with a chronic disease, surgical, and drug addiction history denied. He refers to abdominal trauma 20 years ago while playing soccer. Current condition: started 5 months ago with increased volume and pulsatile tumor in the left inguinal region and in the hypogastrium without pain, 6/10 reported sudden pain 4 days prior to admission, USG of soft tissues showed a probable iliac artery aneurysm, for which he was referred to this unit. He is assessed by the angiology service and his admission is decided. On physical examination, the abdomen was soft, at the hypogastrium level a pulsatile tumor was palpated, without being able to clearly define the extension, adhered to deep planes, not painful on palpation, normal peristalsis, without signs of peritoneal irritation. Lower extremities with arterial integrity pulses 2/2 of good intensity bilateral ITB 1 (Fig. 5).

Figure 5 Tomography angiography showing a giant left iliac aneurysm (LAI), occupying the entire pelvic floor without involvement of the hypogastric artery. A: transverse plane. B: coronal plane. C: sagittal plane.
Angiotomography with 3D reconstruction confirms the presence of a left common iliac aneurysm with a neck length from the level of the aortic bifurcation of 40 mm in diameter and a diameter of the iliac artery of 13 mm at the proximal level, maximum diameter of the aneurysm is 90 mm with a length of 120 mm that ends at the bifurcation of the external and internal iliac artery without dilation of the hypogastric artery, external iliac distal neck of 11 mm. He is taken to open surgery since the iliac angles are 95 degrees, he does not meet the criteria for endovascular therapy due to anatomy. Prior asepsis and tracheal intubation, infra-umbilical midline incision, a giant 9-mm aneurysm is identified that occupies the entire pelvic cavity. Proximal vascular control of the left common iliac is performed, as well as distal control, identification of the hypogastric, which is ligated. An aneurysmectomy of the entire aneurysmal sac is performed, avoiding injury to the ureter and colon. Placement of an 8-mm ringed polytetrafluroethylene graft 4 cm from the aortic bifurcation to the external iliac artery with continuous 6-zero vascular prolene sutures. Control arteriography shows occlusion of the distal graft due to a decrease in the diameter of the left external iliac artery, which is why the graft is extended to the left femoral region with end-lateral anastomosis. Graft patency control arteriography. Abdominal wall bleeding of 500 cc is closed without hemodynamic repercussions, distal pulses present. The patient evolved satisfactorily with good intensity pulses without complications, so he was discharged after 48 hours without complications (Fig. 6).
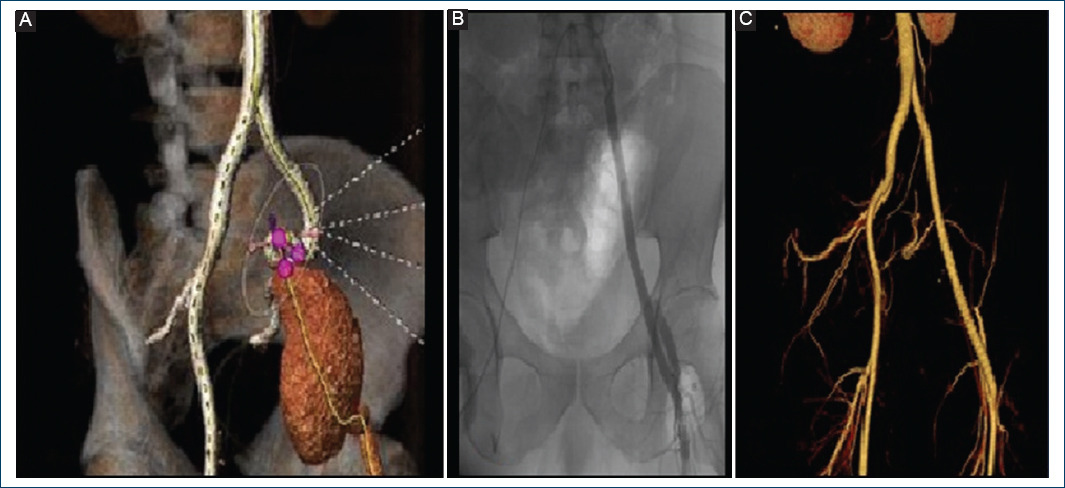
Figure 6 A: 3D computed tomography angiography of AII with a 13-mm proximal neck, a 90-mm maximum aneurysm diameter, and a 12-mm distal neck. B: intraoperative arteriography showing end-lateral iliac femoral bypass with PTEE graft, adequate passage of contrast medium. C: 3D CT angiography at 3 months.
Discussion
The goal of surgical treatment of iliac aneurysm is to prevent rupture. Before the advent of endovascular repair, open surgery was the mainstay of treatment. But with a significant decrease in morbidity and mortality, and fewer complications in patients with iliac artery, endovascular aneurysm repair can be considered as first line therapy2. Iliac aneurysms have certain peculiarities that make open access difficult (location deep within the pelvis, intimate relationships with veins, proximity to the ureter, and difficulty exposing distal branches)3.
AAIC common iliac artery aneurysms are more frequent in females. We present two cases of males, as a history of higher frequency, smoking was present for an average of 15 years, abdominal trauma and abdominal surgery. The giant aneurysm that underwent open surgery, the pathological study did not find any vascular abnormality of the arterial wall. In one case, the patient underwent open surgery because the tortuosity of the iliac veins did not allow endovascular access and the risk of endoleak was greater. In the other 2 cases, the anatomy favored the endovascular approach by presenting less tortuosity and proximal and distal necks.
The mortality rate in cases treated electively with open procedures is 10%. Mortality rises to 33-50% when the aneurysm ruptures. Rupture occurs in 38-51% of cases and characteristically presents with progressive sharp pain, hypotension, and a pulsatile mass in the lower abdomen and inguinal area.
Endovascular repair is the mainstay in the treatment of isolated AAIC, it is safe and feasible. Low mortality rates with excellent technical success rates for primary patency have been observed4. The 3 patients were admitted due to constant abdominal pain in the hypochondria region with irradiation to the lumbar region without loss of pulses with a pulsatile mass assessed by other services with suspicion of urinary and digestive pathologies, for which they underwent tomography with which diagnosis and sent to the service. Tomography angiography was the study of choice to confirm the diagnosis. All patients were sectioned and the anatomy of the iliac region was analyzed to determine the best therapeutic option. The reconstruction of the 3D tomography allowed to know more about the characteristics of the aneurysms.
Table 2 Anatomical features of common iliac artery aneurysms
| Patient | Aneurysm | Proximal neck (mm) | Longitud del aneurisma (mm) | Distal neckl (mm) | Maximum diameter of the aneurysm (mm) |
|---|---|---|---|---|---|
| 1 | Left | 13 | 80 | 11 | 36 |
| 2 | Right | 13 | 65 | 12 | 32 |
| 3 | Left | 13 | 120 | 11 | 90 |
Table 3 Technique and type of material used for iliac artery aneurysm repair
| Paciente | Technique | Type of material | Amount | Measures | Discharge (hours) |
|---|---|---|---|---|---|
| 1 | Endovascular | Covered Stent | 4 | Three: 16 x 38 mm One: 10 x 50 mm | 48 |
| 2 | Endovascular | Overed Stent | 1 | 13 x 96 mm | 48 |
| 3 | Open | Graft PTFE | 1 | 8 mm, linear ringing of 40 cm | 96 |
The Endovascular technique is associated with reduced surgical trauma, shorter hospital stay and less blood loss, with faster postoperative recovery. Endovascular repair of these aneurysms has recently become the preferred form of treatment, when adequate anatomy exists for endovascular repair. Endovascular treatment of AAIC aneurysms has become the first-line treatment whenever anatomical conditions allow it. It should be noted that proximal and distal necks (> 1.5 cm in length) without mural thrombus are necessary to have a correct landing zone.
In addition, the diameter of the proximal seal zone is usually significantly larger than the diameter of the distal seal zone, which in most cases is the external iliac (hypogastric) artery. When treating AAIC by any method, strategies to preserve pelvic circulation should be considered. The natural history of internal iliac (hypogastric) artery aneurysms is still unclear, but several authors recommend repairing these aneurysms when the diameter exceeds 3 cm, since the risk of rupture in such cases is 14-31%. The loss of one or both internal iliac arteries exposes the patient to a greater risk of pelvic ischemia such as colon ischemia, buttock claudication, and erectile dysfunction5.
In all three cases we knew the importance of preserving the hypogastric artery; in all cases we opted for its occlusion since we had the other healthy hypogastric branch, the age of the patients, and the degree of collateral circulation. The follow-up of the outpatient clinic did not present data of gluteal or colon spinal cord ischemia. Only in one case was the diameter of the hypogastric artery considered to be at risk of endoleak, so it was excluded with coil placement. Some authors who do not have access sites to treat endoleaks in endovascular repair sites for AAIC have opted for other alternatives such as a direct percutaneous transgluteal approach. Lumbar branches are located, which is embolized with coils, thus obtaining closure of the aneurysmal sac6.
Currently, there are more modern treatment options to avoid occlusion of the hypogastric arteries in AAIC and it is the branched stents which are only indicated when the patient has a landing site that can help preserve pelvic flow. The patients did not have diameters that would allow the deployment of a branched endoprosthesis at the iliac level. The evolution of the patients is usually to complications such as rupture. There is a rare case reported in the literature of a large and isolated AAII that experiences spontaneous thrombosis without surgical intervention (diameter 5.5 cm from the internal iliac artery), a rare presentation that has not been previously reported in the literature7. The early diagnosis of the 3 patients and the selection of the best therapeutic option allowed a good technical result.
Conclusions
Common Iliac Artery Aneurysms occur in a very low percentage, palpation of a pulsatile mass and pain in the hypochondrium can guide the diagnosis but in a patient with an abdomen with a large adipose panniculus it is difficult. Late detection is associated with rupture of the aneurysm with a very high mortality. Treatment is very complex, surgical or endovascular resolution requires adequate parification to obtain good results.











 nueva página del texto (beta)
nueva página del texto (beta)