Introduction
Cancer is a global health-care issue, in 2018 the World Health Organization (WHO) estimated that cancer was the first or second leading cause of death in 91 of 172 countries1. At present, it is the third cause of death in Mexico2. Seventeen million cases of cancer and about 9.5 million cancer-related deaths were reported in 2018 worldwide.
Genitourinary (GU) malignancies include prostate, bladder, kidney, testis, and penile cancer. They represent 13% of the total incidence of new neoplasms and 8% of cancer-related deaths globally1. Prostate cancer is the most common cancer diagnosis in males in 105 countries. In Mexico, it is the leading cause of cancer-related death accounting with 8.3% and it represents the most common neoplasm in males with an estimated incidence of 13.1%. Testis cancer is the third most common cancer in Mexican males (6.5% of total of new cases), in contrast, it was reported to be in the 29th position in cancer worldwide incidence in 2018 (0.4% of new cases reported)1,3.
Most GU neoplasms have different treatment alternatives that ideally should be discussed by a multidisciplinary team. This group of experts has a broad understanding of the disease and aims to reach the best individualized treatment decision for the patient. It requires the participation of several medical fields for designing adequate treatment plans in specialized units recognized as Urologic Oncology Clinics (UOCs). The multidisciplinary tumor board (MTB) advantages include decisions based on evidence, greater accuracy in diagnosis, patients access to clinical trials, improved communication between specialists, cost-effective medical care, and an academic environment4.
A systematic review which included 51 studies evaluated the effects of these meetings on oncological outcomes. The analysis revealed a positive impact on survival among patients with colorectal, head and neck, breast, esophagus, lung, and GU tumor5.
In 2005, the first article published about the results of MTB in GU cancers showed no changes in clinical management in 98% of discussed cases6. The urologic oncology field has evolved dramatically in the past years with the approval of new diagnostic procedures and novel treatments. In contrast to previous data, in 2011, a prospective study included 269 patients with GU neoplasms found modifications in the diagnosis and treatment in 38%, the most common changes related to treatment in patients with bladder cancer (44%), followed by kidney cancer (36%), testis cancer (29%), and prostate cancer (22%)7. Another study showed that adjustments were more likely to occur in patients with advanced disease (p ≤ 0.05)8.
Despite the availability of international guidelines that establish the ideal requirements for UOC9 and multidisciplinary teams, these recommendations may not be appropriate or feasible for low- and middle-income countries (LMICs). In general, these nations struggle with poor health-care regulation, uncoordinated initiatives, and limited capital. In addition, every country faces unique and diverse geographical, political, and economic barriers and physicians need to cope with them to provide high-quality cancer care10.
In Mexico, the actual situation of UOC and GU-MTB is unknown. The study aimed to evaluate the current status of UOC, determine the existence of GU-MTB, and define the resource disparities among different centers in Mexico.
Materials and methods
This was a cross-sectional study from June 2017 to June 2018, members of the Mexican Society of Oncology (SMeO) were recruited to participate in an online survey on the SurveyMonkey® platform. It was designed and revised by the Mexican Cooperative Research Group in Oncology-GU Tumors Section (GCIMO-GU).
First, a pilot survey was carried out with committee members (n = 9), and then, through the SMeO database, it was sent through e-mail in duplicate to all members. The basic questions included general information about the respondent: institution affiliation, medical specialty, and health system sector (public and private sectors were included to be inclusive of all health-care practices) (Appendix 1). MTB was defined as a periodic meeting where a group of physicians discusses the diagnosis and treatment options for a specific patient from each center. Regarding to UOC and GU-MTB, the questions were focused on the type of GU tumors discussed, the percentage of cases presented, medical specialists involved in the sessions, and the diagnostic and therapeutic procedures available. We included questions about the availability of a reproductive biology department and assessment of patients for sperm cryopreservation. Finally, we incorporated a question about how important an MTB is for a multidisciplinary approach in GU tumors for the practicing physician (essential, very important, important, unimportant, and not necessary).
Descriptive statistics were used to analyze the data collected using means, medians, and relative and absolute frequencies.
Results
The questionnaire was sent by e-mail to 1600 members of SMeO, 31 medical specialists focused on GU cancers responded to the survey. According to their medical specialty: 17 were medical oncologists (55%), 6 were urologists (20%), 5 surgical oncologists (16%), and 2 radiation oncologists (7%). In relation to the health-care system, 19% of medical specialists and 20% UOC belong to private medicine and the rest to the public sector.
The 31 surveyed physicians were affiliated to 20 different UOCs (n = 20) distributed in 8 of 32 states in Mexico: Mexico City, State of Mexico, Jalisco, Nuevo León, Puebla, Querétaro, Chihuahua, and Guanajuato (Fig. 1). The vast majority of centers were located in Mexico City (40%), followed by Jalisco with 20%, State of Mexico with 15%, and the remaining with 5% each.

Figure 1 Geographical distribution of the urologic oncology clinics in Mexico. The number corresponds to the available clinics by each state. The asterisks (*) indicate private medical centers.
Ten of the 20 institutions reported to having a GU-MTB. These 10 centers were distributed in only five states in the country: Mexico City (50%), Jalisco (20%), State of Mexico (10%), Nuevo León (10%), and Guanajuato (10%) (Fig. 2). Only one of them was in the private practice sector.
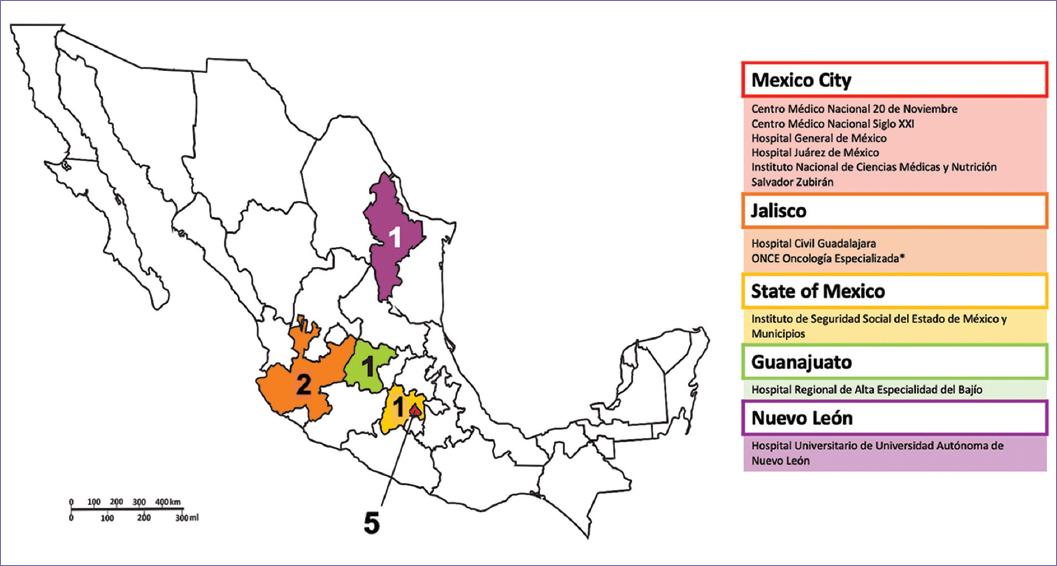
Figure 2 Geographical distribution of the urologic oncology clinics in Mexico with genitourinary multidisciplinary tumor boards (GU-MTBs). The number corresponds to the available clinics with GU-MTBs by each state. The asterisks indicate private medical centers.
Considering medical oncology, urology, and radiation oncology as minimal requirements for a multidisciplinary discussion, this was present in 90% of UOC with MTBs. About 40% of the UOC reported that less than a half of the cases seen in the clinic were presented in the MTBs. About 90% of the MTBs discussed all GU malignancies; only one center reported that they exclusively discuss kidney cancer cases.
Pathology and radiology department support during the sessions were reported in 70% and 60%, respectively. Only 2 centers (20%) had specialists in palliative medicine and geriatrics involved. None of the centers include nursing personnel, social work staff, and neither research coordinators in the sessions (Table 1).
Table 1 Medical specialties involved in multidisciplinary tumor boards (MTBs)
| UOC with MTBs | Medical specialists in the tumor board | |||||
|---|---|---|---|---|---|---|
| U | MO | RO | P | Rx | Others | |
| Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán | ✓ | ✓ | ✓ | ✓ | ✓ | Geriatrics, anesthesiology, nephrology. |
| Centro Médico Nacional 20 de Noviembre | ✓ | ✓ | ✓ | ✓ | ✓ | Surgical oncology |
| Hospital Regional de Alta Especialidad del Bajío | ✓ | ✓ | ✓ | X | X | |
| Centro Médico Nacional Siglo XXI | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Hospital General de México | ✓ | ✓ | ✓ | X | X | Palliative medicine |
| Hospital Juárez de Mexico | ✓ | ✓ | ✓ | ✓ | ✓ | |
| ONCE Oncología Especializada | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Instituto de Seguridad Social del Estado de México y Municipios | ✓ | ✓ | ✓ | ✓ | ✓ | Nuclear medicine, palliative medicine, geriatrics, clinical nutrition |
| Hospital Universitario de la Universidad Autónoma de Nuevo León | X | ✓ | ✓ | X | X | |
| Hospital Civil Guadalajara | ✓ | ✓ | ✓ | ✓ | X | |
*UOC: urologic oncology clinics; U: urology; MO: medical oncology; RO: radiation oncology; P: pathology; Rx: radiology; ✓: yes; X: no.
Diagnostic imaging availability in centers with or without GU-MTBs is described in table 2. Among institutions without GU-MTBs, 30% lacked bone scan, 10% did not have magnetic resonance, and immunochemistry was not available in one-third of the centers. In relation to therapeutic procedures, all UOCs with MTB could offer radiotherapy to their patients. On the other hand, 30% of UOCs without a tumor board lacked radiotherapy. There was limited access to reproductive biology assessment and sperm cryopreservation in all centers.
Table 2 Diagnostic and therapeutic procedures in centers with and without tumor board
| Diagnostic and therapeutic procedures | With tumor board (n = 10) | Without tumor board (n = 10) |
|---|---|---|
| Bone scan | 10 | 7 |
| Computed tomography (CT) | 10 | 10 |
| Magnetic resonance (MR) | 10 | 9 |
| Positron emission tomography (PET) | 6 | 4 |
| Tumor markers* | 10 | 10 |
| Immunohistochemistry (IHC) | 10 | 7 |
| Radiation therapy | 10 | 7 |
| Reproductive biology assessment | 6 | 2 |
| Sperm cryopreservation | 4 | 1 |
*The tumor markers included in this question were: PSA: prostatic-specific antigen; LDH: lactate dehydrogenase; AFP: alpha-fetoprotein and BHCG: beta-human chorionic gonadotropin.
Finally, the perceived relevance of having these multidisciplinary sessions by physicians surveyed was reported as follows: 61% considered it essential in their clinical practice, 29% considered it very important, 7% important, and 3% considered it unimportant (this last group of physicians work in clinics without MTB).
Discussion
A multidisciplinary strategy is key for improving outcomes in GU neoplasms. This has been recommended by ASCO and other international guidelines and has become the model of care in several countries as the United States, Australia, and Canada11. This approach offers advantages such as standardization of diagnostic procedures and treatments, effective communication between medical specialists, and improvement in patients outcomes12. Nevertheless, its implementation in LMICs remains challenging and must be individualized according to the country resources.
Mexico is the 14th largest country in the world with an estimated population of 120 million people. It covers an area of 1.96 million km2, this means it is 4 times bigger than France or Spain and it comprises 32 states13. Our study identified 20 UOCs. This situation implies that there is one clinic specialized in GU tumors for every 5.8 million people. If we only count the centers with a GU-MTB (n = 10), it would represent one UOC for every 12 million inhabitants. In addition, according to the 2018 GLOBOCAN data, in Mexico, the estimated number of new cancer cases was 190,000/year, and 20% of these tumors constitute GU neoplasms. This gives an estimate of 38,000 new urologic oncology cases per year, which implies that there is one UOC for every 1900 new GU cancers cases per year in our country according to the survey.
This phenomenon is further aggravated, when we analyze the amount of UOC by square kilometer (km2) in the national territory. Considering that the 20 centers identified were located in only 8 of our 32 states: one clinic for every 98 000 km2. The distribution of the centers is not equal in the country territory. Most of the clinics are centralized and established in three states (Mexico City, Jalisco, and State of Mexico), accounting for 75% of the total of UOC. This condition illustrates disparities in access to the health-care system for Mexicans and shows the geographical barriers for patients diagnosed with GU tumors in our nation.
Most UOCs identified are in the public practice sector, where the patient burden has led to tumor type allocation to a particular oncologist. A minority of the centers participating were from the private health system. This phenomenon is a reflection that oncologists in private practice are mostly solo practitioners engaged in seeing general oncology without the support of a multidisciplinary team. We need to recognize that most UOCs with GU-MTBs are third-level health care institutions which are a privileged minority. Most Mexican patients with GU malignancies are still seen in the first or second level health care institutions that lack a structured oncology department. Medical oncologists struggle to provide care by themselves to all sorts of malignancies in the absence of a multidisciplinary team.
LMICs physicians need to provide high-quality care adapting their decisions to their environment resources, and this may also vary inside the country. Heterogeneity in access to medical services or tests is clearly seen in this survey. This disparity is more palpable when comparing UOCs with and without a GU-MTB. Nuclear medicine imaging tests such as PET and bone scan, radiation therapy, and IHC are often unavailable and physicians need to take clinical decisions accordingly.
Finally, there is a profound deficit in the oncofertility field, including the assessment of patients by a reproductive biology specialist and sperm cryopreservation availability in all UOCs. This is especially important for young adults with highly curable neoplasms such as testicular cancer. It was also concerning that our survey revealed, the low participation of geriatrics and palliative care specialists in MTBs. This is particularly worrisome, in a setting, where most patients with bladder and prostate cancer are over 65 years old and have several comorbidities.
In the evaluated UOC, there was a generalized lack of nursing, social work, and research staff, this contrasts with the reality of MTB in high-income nations and is a reflection of the scarce workforce medical institutions in LMICs. This compromises the adequate navigation of the patients, support with referrals, and timely evaluation for inclusion in clinical trials.
As a survey, this report has a participation bias. Although the survey was conducted through the SMeO, some specialists are not active members, some institutions are not in continuous communication with the society, and some members might have decided not to answer the survey. We also need to acknowledge a recall bias, answers were based on the specialist experience and not on reported and audited resources of each institution. Our survey was designed by the group of experts in the Mexican Cooperative Research Group in Oncology-GU Tumors Section, however, it is was not a validated tool. Our results constitute the first approximation to the reality of MTBs in Mexico, nevertheless, it was a 1-time survey, and repeated questionnaires will be needed to address the changes in GU malignancies care in our country overtime.
As a national society, we are aware and committed to continue updating the data. It is important to highlight that the majority of physicians surveyed consider MTBs as an essential and very important tool in their daily practice. Moreover, this is reflected in the fact that they present most of their cases in tumor boards.
This study represents a call to action for the Mexican Cooperative Research Group in Oncology, GU Tumors Section. We have successfully identified centers where multidisciplinary teams are organized for the care of patients with GU malignancies and the location of institutions with GU-MTBs. Now, we must move forward to the next level! It is essential to create networks between centers, to counteract local deficiencies, and strengthen patient referral in and out of the clinical trials setting. We need these UOCs to become the ideal setting for patient care, as a group we are committed to delineate a list of minimal requirements and operation recommendations for GU-MTBs. Finally, the SMeO must create national awareness and promote the governments commitment to this unmet need.
Conclusions
This study is the first description of the current status of UOCs in Mexico. There are 20 centers with these clinics in the country, however, only 50% of them have a MTB for the discussion of GU cancer cases before treatment. There is a great centralization of specialized medical care, with only 8 of 32 states with organized clinics, and most of them are localized near Mexicos capital. Medical resources available are heterogeneous among clinics and are particularly scarce among those lacking MTBs. In addition, opportunities for fertility preservation are very limited. The disparity among centers is shown by the absence of nuclear medicine studies, unavailability of radiation therapy, and lack of pathology techniques such as immunohistochemistry in some centers; this is an important fact that could impact patient outcomes. The uneven geographical distribution of UOCs and the unequal availability of medical resources reflect an evident disparity in access to health-care services in Mexico.











 nueva página del texto (beta)
nueva página del texto (beta)


