Introduction
The salivary glands are divided into two groups, the major salivary glands, which include parotid, submandibular, and sublingual glands, and the minor found in the aerodigestive tract. There are between 600 and 1000 minor salivary glands that measure between 1 and 5 mm in diameter; they are found in greater concentration in the oral cavity and oropharynx and less in the nose, paranasal sinuses, pharynx, and larynx. Salivary gland tumors are usually benign, and most of them occur in major salivary glands. Myoepithelial carcinoma is a rare tumor in the salivary glands, most of them are benign. Hereford, we present a rare case of malignant myoepithelial carcinoma located in the maxillary sinus.
Case report
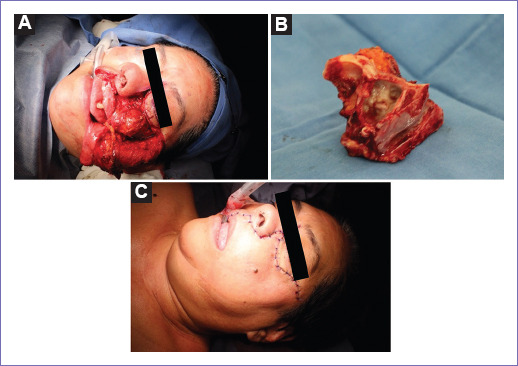
A 64-year-old female with a medical history of resection of a hard palate tumor 30 years ago, apparently benign, presents to the clinic with an 8-month history of progressive pain and swelling of the left maxilla, attributed to a dental prosthesis, receiving antibiotic treatment. Extraction of the upper left premolar is done without improvement. Subsequently, an increase in the upper left gingiva volume was noticed, biopsied, and an odontogenic tumor was reported. Examination revealed a bulging of the left hard palate and an increase in the upper gingiva volume of approximately 5 × 5 cm (Fig. 1). No lymphadenopathy was palpated.
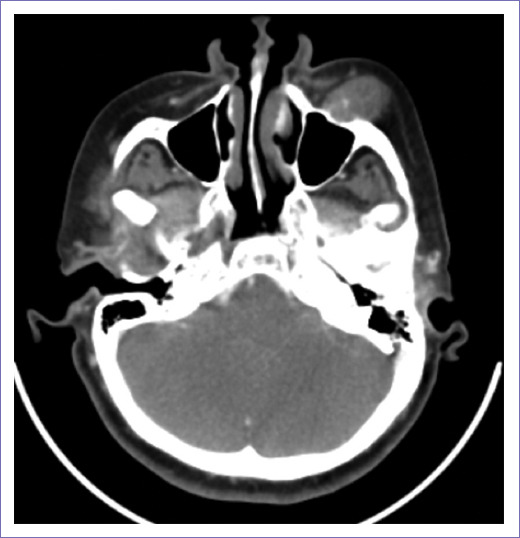
A face CT scan revealed a heterogeneous left maxillary tumor with bone destruction, which measured 34 × 28 mm, extending into surrounding soft tissue and masticator space, with an invasion of the hard and soft palate (Fig. 2). No adenopathy was identified. A left infrastructural maxillectomy was performed. The tumor was resected entirely, a solid tumor was identified, measuring approximately 4 × 4 cm, with intimate contact with the orbit floor, without infiltrating it. Furthermore, infiltration to the hard palate, up to the midline, was observed (Fig. 3 A, B, C). The post-operative period was uneventful, and she was discharged on post-operative day 4. Final histopathological examination reported a myoepithelial maxillary carcinoma. Immunohistochemical staining revealed positive for S100, calponin, and P63 negative. Adjuvant radiotherapy, with 60 Gy, was administered.
Discussion
The salivary glands are divided into two groups, the major salivary glands, which include parotid, submandibular, and sublingual glands, and the minor found in the aerodigestive tract. There are between 600 and 1000 minor salivary glands that measure between 1 and 5 mm in diameter; they are found in greater concentration in the oral cavity and oropharynx and less in the nose, paranasal sinuses, pharynx, and larynx. These originate from the ectoderm of the upper respiratory tract around the 12th week of gestation. The glands are made up of parenchyma, with secretory units and associated ducts, and connective tissue stroma that divides the glandules into lobules. These are exocrine glands secreting saliva from their acinus toward the epithelial surface. The myoepithelial cells surround the acinus, and its contraction triggers the secretion of saliva into the epithelium1.
Salivary gland tumors are rare and primarily benign; only about 20% are malignant. The annual incidence of salivary gland cancer is 0.5-2/100,000. Although these tumors can occur in major or minor salivary glands, most of them occur in major salivary glands. It is considered that the smaller the salivary gland in which the tumor occurs, the more likely it is to be malignant2. Up to 80% of tumors in minor salivary glands are malignant, while only 25% of those are in the parotid gland1. In general, minor salivary gland tumors appear as submucosal tumors, which later ulcerate; since most of these are found in the oral cavity. Data suggestive of malignancy include nerve involvement, which can be evident with facial palsy, accelerated growth, fixation to deep tissue, and cervical lymphadenopathy2.
Minor salivary glands cancer represents 2-4% of all head-and-neck cancer and 10-15% of all salivary glands neoplasms1. The most common type of cancer in the minor salivary glands is adenoid cystic carcinoma followed by mucoepidermoid carcinoma2. Myoepithelioma is a rare tumor, representing 1% of all salivary gland tumors; 90% are benign3,4. The malignant variant represents only 0.1-0.45% of salivary gland neoplasms3. Myoepithelial carcinoma is not exclusive of salivary glands, it can also arise from skin and soft tissue. About 15% of these tumors arise in minor salivary glands5. This neoplasm was first described by Yang et al. in 1975 and was included as a separate clinicopathological entity by the World Health Organization in 19916. It occurs more frequently in adults over 50 years of age, without an apparent gender predilection; although a recent systematic review reports a higher frequency in females3,5,7. In general, they are solid tumors, measuring from 2 to 10 cm, firm, nodular; necrosis or cystic degeneration areas may be present1. The most common location is in the palate6. Microscopically, it has infiltrative, destructive growth into the adjacent salivary gland and soft tissues. The nodules of tumor cells are usually separated by fibrous stroma. Four types of cells can be found in myoepithelioma; usually, more than 1 type is found, including epithelioid, plasmacytoid, spindle cells, and clear cells1. The most frequently found cell is the epithelioid followed by clear cells6. It is designated as a cell type when more than 75% of the tumor cells are one type. Myoepithelial carcinomas may arise from pre-existing benign lesions or occur de novo. In a study made by Savera et al., with 25 patients, it was determined that 75% of the cases were de novo, while 25% of the tumors arise from benign tumors7. Myoepithelial carcinoma that arises from benign lesions is generally low grade, while de novo is generally high3.
The diagnosis is made by confirming exclusive myoepithelial differentiation and evidence of malignancy – infiltrative growth and perineural invasion6,7. Atypia may or may not be present7. Myoepithelial differentiation is not uncommon; however, tumors that are formed only by myoepithelial cells are rare3,7. The distinction of malignancy may be difficult; the presence of atypia, cellular pleomorphism, >7 mitotic figures per 10 high-power fields, necrosis, and invasive patterns are some features that determine malignancy3. Immunohistochemical markers are used to distinguish from other neoplasms. The markers that have the best sensitivity are S100 and vimentin, although others have also been used, such as calponin, p63, CD10, and anti-keratin antibodies6,7. More than 10% of positive Ki-67 is diagnostic for malignancy3,6.
When a salivary gland tumor is suspected, radiological investigations may be employed to delineate tumor location. Ultrasound is used for parotid and submandibular glands, but it is not helpful for minor salivary gland tumors. Magnetic resonance (MR) is considered more valuable than computerized tomography in predicting malignancy and detecting small tumors, for they have an intermediate to low signal in MR. It is also better in detecting extension, marrow infiltration, and perineural spread. The use of PET scans is still being evaluated. As mentioned before, the diagnosis is confirmed by histopathological examination. Fine-needle aspiration cytology has a sensitivity of 85% and a specificity of 99%2.
A myoepithelial carcinoma usually presents as a slow-growing, painless mass3. These symptoms may be associated with surface ulceration and bleeding6. Infiltration to adjacent tissues may cause facial palsy, lip or lingual numbness, dysphagia, and pain, depending on the location. Malignant lesions are more likely to be symptomatic than benign ones. Lymph node involvement may be present. Since it is an uncommon tumor, the prognostic factors are still under investigation. Some potential prognostic factors include clinical stage, site, and size of the tumor, proliferative activity, and invasion into the surrounding tissue. Although no definite histopathological feature correlates with tumor behavior3,7, it has been seen that overexpression of Ki-67 and p53 confers poor prognosis since recurrence and metastasis are more frequent3. Spindle cell subtype has an increased risk of lymphatic and distant metastasis. It is not unusual that this disease's metastasis presents years later, with reports up to 43 years after initial diagnosis3. Spreads to lungs, spine, brain, skin, kidney, ribs, scalp, and bone marrow have been reported3,6.
There is minimal experience in treating this disease; there are currently no guidelines to guide the treatment. Surgery is the mainstay of MC's management3,6, with wide surgical margins in more aggressive tumors3. Neck dissection should only be done if there is proven cervical lymph node involvement6. Adjuvant radiotherapy is currently under investigation: a recent systematic review reports less locoregional recurrence, but no impact in overall survival5. It is generally recommended for high-grade tumors and incomplete resection, perineural invasion or soft-tissue infiltration. It is also recommended for recurrence after complete surgical resection3,6.
Prognosis is given by the complete surgical resection, which is the only curative treatment6. Tumor size and mitotic index have also been seen to affect recurrence5. Tumors with p63 and Ki67 overexpression have also presented recurrence and metastasis more frequently8. In the present case, p63 was negative, while Ki67 and p53 were not determined. We can imply that the patient has a good prognosis.
Six cases, including this one, have been reported in the literature (Table 1). All of these cases had exclusive myoepithelial differentiation. About 50% were women, between the ages of 38 and 67, with an average of 50 years. Most of them presented with dull pain and swelling in the cheek. All of them underwent surgical resection. Three of them presented recurrence, one of which died9, but we have no information on the other two patients10,11. Only one patient received chemotherapy9 and three radiotherapy4,9.
Table 1 Myoepithelial carcinoma case reports
| Author | Age | Gender | Clinical presentation | Treatment | Recurrence | Treatment of recurrence | Outcome |
|---|---|---|---|---|---|---|---|
| Hata et al. | 47 | F | Cheek swelling and pain | Surgical resection | Yes | RT | Survival |
| Zhou et al. | 41 | F | Nasal obstruction | Surgical resection + Chemotherapy | Yes | RT | Death |
| Albergoni et al. | 44 | M | Facial asymmetry | Surgical resection | - | - | - |
| van Roggen et al. | 67 | M | Cheek pain | Surgical resection | - | - | - |
| Savera et al. | 38 | M | - | Surgical resection | Yes | Death | |
| Present case | 64 | F | Swelling and pain | Surgical resection + RT | No | - | Survival |
Myoepithelial carcinoma is a rare entity that affects salivary glands. The vast majority of them arise in major salivary glands and are usually de novo. It is crucial to know de histopathological and immunohistochemical features to diagnose this disease accurately. The treatment is surgical excision, with wide margins. Prognosis is determined by this and by histopathological features. Radiotherapy is under investigation, but it does not seem to improve prognosis significantly. Only six cases, including this one, have been reported in the literature; half of them are female, and also, half of them presented recurrence.
It is essential to correctly identify and treat this disease to improve the prognosis.











 nueva página del texto (beta)
nueva página del texto (beta)